Determining Your Tolerance to Alpha-gal
Part I: First Steps
A Guide for People with Alpha-gal Syndrome
Before You Get Started…
Your physician needs to advise you as to what’s best for you, based on your clinical history, test results, and other factors. Please seek a physician’s advice before attempting to determine your alpha-gal tolerance level.
If you are newly diagnosed with alpha-gal syndrome (AGS), you might not know how much alpha-gal it takes to cause you to react. There are no straightforward guidelines for determining your unique level of tolerance to alpha-gal, but some foods, drugs, and other products are more likely to affect you than others. The information here is based on the experiences of people with AGS. It is not medical advice, and it is not designed to replace your physician’s advice or common sense or to tell you exactly how to proceed. Everyone’s alpha-gal journey is different, and you will need to personalize the suggestions offered here to meet your own, unique needs.
Before you try to figure out your tolerance level, there are a few things you need to understand about AGS.
Expert Dr. Scott Commins answers the Two Alpha Gals question: Where is the best place to start after alpha-gal syndrome diagnosis?
For more Common Questions with Dr. Commins see the Two Alpha Gals website.
Not a Red Meat Allergy
Many people, including physicians, think that alpha-gal syndrome is a red meat allergy. It is not. AGS is an allergy to galactose-alpha-1,3-galactose (alpha-gal). Alpha-gal is found in the tissues, cells, and fluids of non-primate (and some primate) mammals (1, 58). Red algae (71) and many other organisms, most of which we don’t eat, also make alpha-gal (8, 58, 74, 104, 105, 107, 108, 110, 111, 112). Products made with ingredients derived from mammals and other organisms that express alpha-gal can contain alpha-gal, too (6, 57).
In addition to mammalian meat, the following can contain alpha-gal:
- Mammalian organs, tissues, blood, and other fluids, including amniotic fluid (57, 6, 58)
- Milk and dairy products (57, 6,)
- Gelatin (28, 42 103, 57, 6)
- Foods containing mammalian byproducts (57, 6)
- Foods processed with, or cross-contaminated by, mammalian byproducts (57, 6)
- Flounder eggs (26, 104)
- Carrageenan (54,57)
- Drugs, biologics, and other medical products made with mammalian byproducts or carrageenan (28, 42 103, 57, 6)
- Personal care products made with mammalian byproducts or carrageenan (57)
- Household products made with mammalian byproducts or carrageenan, like some cleaning products and air fresheners (57)
- Pet saliva and dander (57)
- Fumes (airborne droplets of fat) from cooking meat (57)
- Various other products, including some unexpected industrial products, like drywall
- Various other organisms (8, 58, 74, 104, 105, 107, 108, 110, 111, 112)
Products that contain alpha-gal may be:
- Even riskier for us than red meat, like the cancer treatment cetuximab (30) and gelatin-based volume plasma expanders (91) or
- Tolerated by some of us (57, 6) or
- Tolerated well by most people with alpha-gal syndrome (57, 6)
We do not know how much alpha-gal there is in most products made with mammalian ingredients. Some may not even contain alpha-gal. Until more information is available, most of us rely on a combination of expert opinion, published accounts of patients’ reactions, anecdotal reports, and our own experiences to guide us.
Some Exposures Are Riskier Than Others
Some foods and medical products are extremely risky for people with alpha-gal syndrome and may cause reactions even in people who tolerate mammalian meat. Examples include:
- Pork kidneys (24,59)
- The cancer treatment cetuximab (30)
- Gelatin-based plasma volume expanders (91) (not used in the U.S. much, if at all)
Other foods and other products are tolerated by many of us, but not by a significant percentage of us, like:
- Milk and other dairy products (57)(6)
- Gelatin in foods (most of us can react to gelatin in some medical products) (57)(6)
- Gelatin in gelcaps
- Carrageenan (57)
- Whey (57, 115)
Only a minority of us react to many foods and medications that contain trace amounts of mammalian byproducts, but for those who do react to them, reactions can be severe. The charts below provide some information about relative risks, to the extent we understand them.
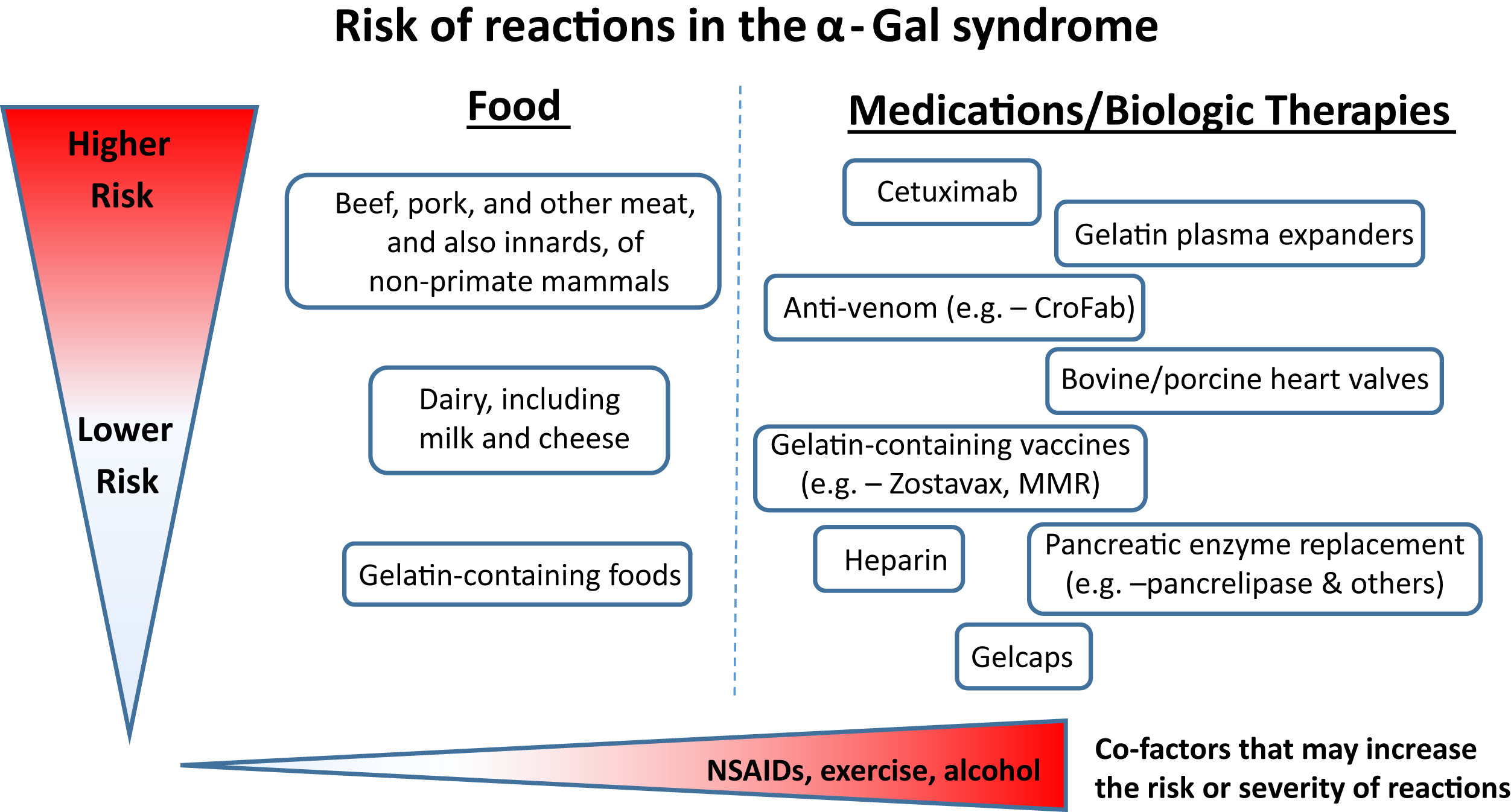
Figure 1. The risk and also severity of reactions in the α-Gal syndrome relate to the amount of the oligosaccharide that is present in food, drugs, or other therapeutics. The route of administration is relevant to the speed at which reactions occur; that is, intravenous administration is associated with rapid reactions, whereas oral ingestion has delayed onset. Cofactors such as NSAIDs, exercise, and alcohol can be additional risk modifiers. This schematic reflects clinical experience, as well as challenge studies and laboratory investigations. CroFab, Crotalidae polyvalent immune Fab; MMR, measles, mumps, and rubella; NSAID, Nonsteroidal anti-inflammatory drug.
Reproduced from: Platts-Mills TA, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-Gal syndrome. The Journal of Allergy and Clinical Immunology: In Practice. 2020 Jan 1;8(1):15-23, with permission from Elsevier.
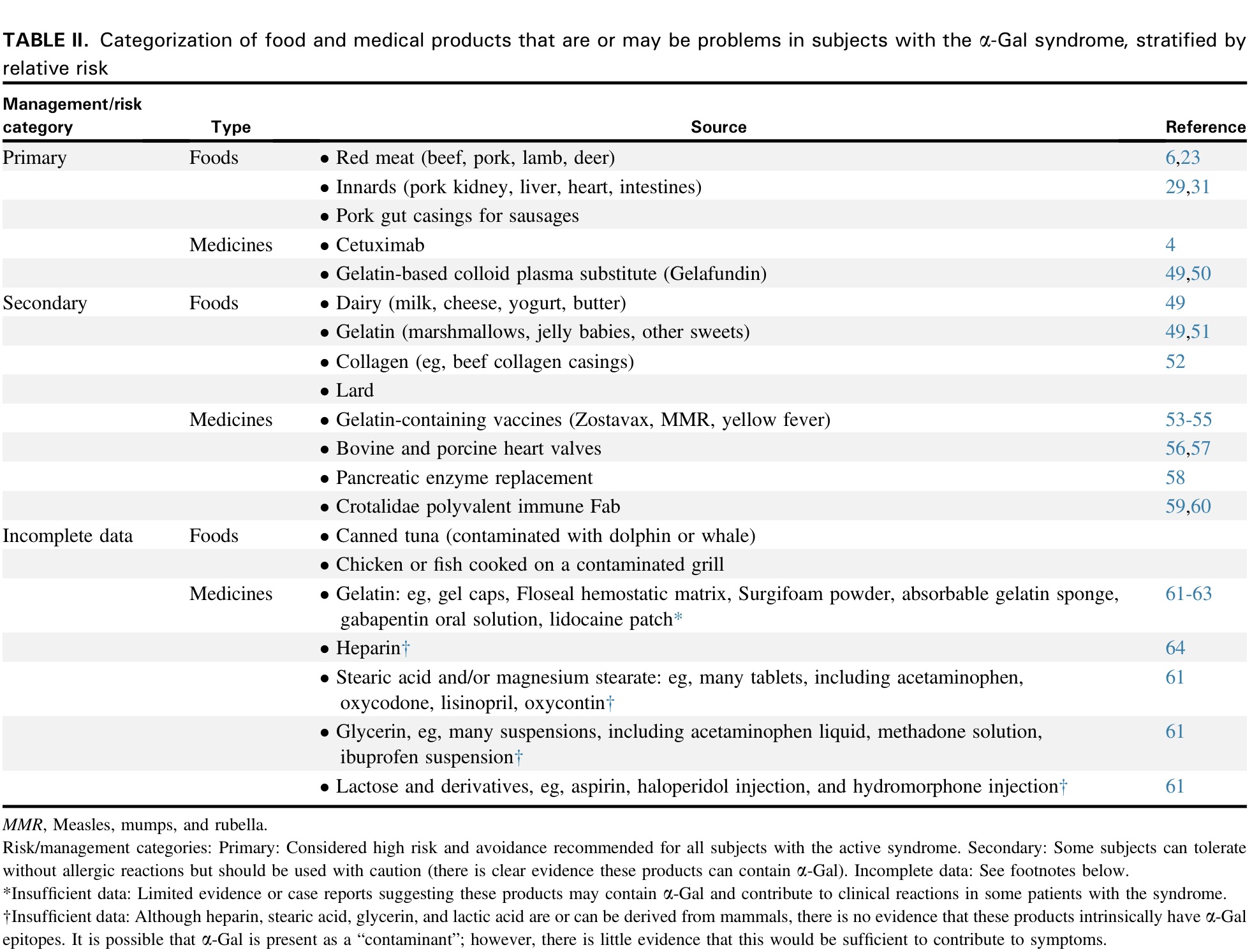
Reproduced from: Platts-Mills TA, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-Gal syndrome. The Journal of Allergy and Clinical Immunology: In Practice. 2020 Jan 1;8(1):15-23, with permission from Elsevier.
Everybody Is Different
The thing about Alpha-gal Syndrome is that reactions seem to be as individual as each of us is. About half of us can eat dairy, some have reactions from carrageenan, some of us react to fumes, but most don’t. And reactions can change over time. People get over fume reactions while others who may never have had them before suddenly develop them. It’s a crazy roller coaster ride, but just because we have AGS, it doesn’t define who you are. Here, you know you’re never alone, we’re stronger together and here to help. The important thing to remember is to figure out your triggers & avoid them and otherwise do the things you’d normally do as much as possible.
Reactions to alpha-gal vary enormously from individual to individual (57). This means:
- Some people only have to stop eating mammalian meat and organs and avoid some medical products (57).
- Other people need to avoid additional foods, like dairy and gelatin, as well (57).
- Still others cannot tolerate a wide variety of foods, personal care, household, and other products containing only micrograms of alpha-gal (57).
- Some people react to airborne particles of alpha-gal, such as those produced by cooking meat (57).
Alpha-gal Reactions Are Unpredictable & Change Over Time
Whether a reaction occurs to an individual exposure often appears to follow no identifiable pattern for patients. The lack of consistent reactions is, in itself, almost a diagnostic hallmark (57).
An additional point is that some patients with the syndrome may tolerate mammalian meat on occasion with few or no symptoms but have severe reactions on others (57).
Activity, alcohol consumption, and exercise can have profound influence on reactivity (57).
With each individual, reactions to alpha-gal vary from exposure to exposure and often change over time (57). This is due, in part, to co-factors, like drinking alcohol, exercise, the use of NSAIDs (like Advil), illness, infection, stress, lack of sleep, and menses (your period). Recent tick bites can also influence the severity of symptoms. This means:
- You may react differently to the same foods on different occasions. For example, one day, you may eat a steak and feel fine; the next day, you may eat a steak and have a life-threatening reaction.
- If you have wine with a meal or go for a run after eating, you may be more likely to have a reaction.
- If you are lucky, you may become less reactive with time, especially if you avoid additional tick bites.
- If you are less lucky, your reactions may get worse, and you may react to foods that you previously tolerated.
- This often happens after new tick bites.
- For example, you may be able to tolerate everything except mammalian meat and organs. Then after a new tick bite, dairy products start to bother you or you develop fume reactions.
Before I was diagnosed, sometimes I would eat a hamburger and nothing would happen. Sometimes I would eat a hamburger and just get cramps, bloating, diarrhea, and/or occasionally vomiting. Sometimes I would eat a hamburger and my throat would close and I would have hives the size of dinner plates. It was always Russian roulette.
I already had alpha-gal syndrome and could not handle beef, but I could handle dairy. I used to eat Cheez-its and Cheetos all the time. They made great movie snacks! I had no problems with dairy then, that I know of, other than inflammation. Then, I was bitten by more ticks. Less than a month later, I had anaphylaxis from a snack at work one night. Just a handful of Cheez-its caused anaphylaxis within minutes. Shortness of breath, full body hives, migraine, heart pounding, drop in blood pressure, facial flushing, hot sweats and cold chills, diarrhea, and vomiting all simultaneously.
Watch Out for Atypical Symptoms
Some people with AGS who are diagnosed after developing classic allergic symptoms, like hives and anaphylaxis, eventually discover that by avoiding exposure to alpha-gal, symptoms they have had for years, which they attributed to other conditions, clear up. Examples include:
- GI symptoms, including abdominal pain, IBS-like symptoms, bloating, diarrhea, cramping, vomiting, etc. especially at night (6, 57, 84, 92, 116, 117)
- Arthritis (6, 57)
- Pruritis (itching) (6, 57)
- Migraines (patient anecdotes)
- Fibromyalgia (patient anecdotes)
Keep in mind that different alpha-gal exposures can produce different symptoms, for reasons that are not clear. For example, some people have delayed anaphylactic reactions and/or hives after eating red meat; more rapid-onset GI issues after consuming dairy products; reflux when they eat gelatin, etc.
It is possible that some of us suffered from low-level AGS for many years prior to developing the more obvious manifestation that led to our diagnosis. Many of us have been misdiagnosed with other conditions, like IBS, IBD, and gallbladder disease. Some of us have even had multiple unnecessary surgeries. For this reason, if you have any of the above symptoms or other unexplained discomforts, you may want to consider a more restrictive diet (including avoidance of dairy, gelatin, and carrageenan) for a couple of weeks and see if you feel any better.
I go into anaphylaxis if I ingest mammal meats. I end up on the toilet for 2 days if I ingest dairy.
I end up with severe headaches and body pains if I’m ingesting medications that contain mammal. If I’m around fumes of mammal being cooked, I end up with nausea, diarrhea, swollen face and hands, indigestion, headaches, red eyes that are also swollen, and severe body pains. Thankfully I only end up with red and burning skin if I touch mammal meats.
Should I Continue to Consume Dairy If It Doesn’t Bother Me?
We do not routinely include avoidance of dairy products as part of primary avoidance, as 80-90% of patients with AG do note react to milk or cheese. However, published evidence and expert opinion articles indicate that full avoidance of dairy products perhaps should be recommended in patients already avoiding mammalian meat without adequate control of symptoms (57).
…there may be some evidence that patients on a strict avoidance diet could experience anaphylaxis after ingestion of minimal amount of allergen and this has mirrored our overall clinical experience (57).
A big question that requires further research is whether all patients with the syndrome should avoid dairy because of the possible link wth chronic inflammation of the arteries. We also need to better understand the risk of reactions to the wide variety of products that may include small amounts of material derived from mammals. (6)
The argument about a dairy-free diet changes completely if consumption of α-Gal–containing products can contribute to inflammation without giving rise to allergic symptoms. Before the recognition of IgE to α-Gal, the cardiovascular group in Cambridge reported that patients with triple vessel coronary artery disease had a distinct pattern of IgG and IgD specific for α-Gal. In 2018, we reported that there was significantly worse coronary artery disease in patients who had IgE to α-Gal. That study needs confirmation, but it implies that the risk related to IgE to α-Gal is not restricted to subjects who have allergic reactions. If it is true that patients with IgE to α-Gal have an increased risk of atherosclerosis even if they do not have allergic symptoms there are 2 groups of subjects who may need to be advised to go dairy free as well as avoid red meat: First, patients whose symptoms are “controlled” by avoiding red meat and second, subjects who have IgE to α-Gal but have not recognized symptoms related to red meat. The evidence at present is not strong enough to make this as a recommendation, but clearly it is an area that needs more research. (6)
Some people with AGS choose to give up all alpha-gal-containing foods, not just those they conspicuously react to. This is a personal decision that only you, with the advice of your physician, can make. Before making this choice, though, consider these possible trade-offs:
- People on strict alpha-gal avoidance diets are more likely to go on to develop severe reactions to trace amounts of alpha-gal. Keeping dairy in your diet (if you tolerate it) seems to provide some protection against this (57).
- On the other hand, preliminary research suggests a possible link between the consumption of alpha-gal-containing foods and coronary artery disease among people sensitized to alpha-gal (6).
If you don’t know how to weigh these potential trade-offs, welcome to the club! It’s not an easy decision for many of us, and sometimes experts aren’t sure how to advise us, either.
A Note about Drugs & Other Medical Products
I think the overarching advice is that if someone is in the hospital with COVID it is certainly appropriate to let the providers know about allergies, but the focus should be on treating the infection and its complications. In the unexpected chance there is an allergic reaction, the hospital is the right place to be.
There are thousands of drugs and medical products that contain alpha-gal and thousands more for which the alpha-gal content is uncertain. Some are considered very risky for people with AGS; others aren’t a problem for most of us. Even risky medical products may be appropriate when the dangers of NOT using them outweigh the risks of the reactions they may cause. Dr. Wilson’s above advice is relevant for more than Covid. For example, if a rabid animal bites you, your physician may feel that the potential risks of a reaction to a rabies vaccine (administered with safety protocols, such as graded dosing) may be less than the risks of getting rabies (which has a 100% fatality rate) even though the rabies vaccine contains gelatin. Always seek the advice of your healthcare provider when making decisions about which drugs and other medical products to use or not use.
Sorting out your meds
Many of us work with our healthcare providers using a process like this:
- First, make a list of all the drugs and medical products you use, including the names of the drugs, the manufacturers, and the NDC#s.
- Identify which products contain mammalian byproducts or other potential sources of alpha-gal, like carrageenan.
- In many cases, it’s the inactive ingredients that are mammal-derived, and these vary from manufacturer to manufacturer and even lot to lot.
- If your healthcare provider and pharmacist can’t or won’t help you, which is often the case, look up drug ingredients yourself on DailyMed (see below).
- Use the AGI Mammalian Byproducts Database to help you identify ingredients that may be derived from mammals.
- When it is not clear whether a product contains alpha-gal, contact the manufacturer or the Robert Wood Johnson Hospital Drug Information Center (RWJ) for help (see below). Many of us run all our medications past RWJ.
- For products with an established risk, work with your healthcare provider to explore alpha-gal-free alternatives, for example:
- There are alpha-gal-free alternatives to Armour thyroid.
- Some flu shots contain gelatin and others do not.
- See Step #3 for tips on finding alpha-gal-free versions of your medications.
- When alpha-gal-free options are not available, you may be able to have your medication compounded by a compounding pharmacy. See Step #1 for more information,
- In some cases, an alpha-gal-free alternative may not be available or your healthcare provider may feel that the benefits of a medication outweigh the risks of switching to an alternative.
- For products for which there is incomplete data, the decision process can be more nuanced.
- Most of us tolerate gelcaps.
- Most of us tolerate tablets containing magnesium stearate, stearic acid, lactose, and some other mammalian byproducts in tablets. You may not react to these.
- For those who do react to these ingredients, liquid versions of many medications usually do not contain these ingredients.
Emergencies
When medical emergencies require unexpected ER visits or hospitalization, you may want to:
- Be prepared. Keep information about alpha-gal syndrome with you as part of your emergency kit: more info here.
- Share info about your alpha-gal allergy with your doctors and advocate for yourself, but don’t disregard your doctors’ judgment.
- Remember that medications with trace amounts of alpha-gal in them are NOT problematic for most people with AGS.
- Recognize that in an emergency situation, you might NEED a drug or other medical product, even if there is some risk of a reaction. Reactions can usually be managed in a hospital setting.
- If you have trouble getting healthcare providers to listen to you or understand you, ask for a patient advocate.
Step #1
Recommendations for all people with alpha-gal syndrome
The primary advice for newly diagnosed patients with AGS is to completely avoid meat of mammals. In most areas of the U.S. this means beef, pork, venison, and lamb. Internal organs are equally or more able to induce reactions and these should be avoided as well, especially pork kidney…Meat and products derived from other mammals such as bison, buffalo, rabbit hose, and goat should be equally avoided (57).
Virtually everyone with AGS needs to take the following actions.
Food
- Avoid the highest risk foods, including mammalian meats and organs (57)(6).
- Do not eat flounder roe (eggs)(26, 104).
- Be cautious with high-fat dairy, such as ice cream, and large amounts of butter (57).
- Be careful when eating out. Ask if the mammal fat or broth was added to fry oil, gravies, and sauces. (57)
- Make sure your poultry (turkey, chicken, duck) sausages do not have a mammalian gut casing (57); many do. In addition, be aware that collagen casings may also be a problem.
- Read labels before purchasing or consuming foods.
- Take note of whether dairy, gelatin, carrageenan, or “natural flavorings” (which are often beef or pork, especially in savory foods) bother you.
- Your reactions to each may differ from your reactions to mammalian meat.
- For example, some people get hives, angioedema (swelling), or anaphylaxis from meat but diarrhea from dairy and carrageenan and heartburn from gelatin.
- If you miss red meat, try emu or ostrich. Many people think they taste just like beef.
- There are substitutes for just about every mammalian meat product you might miss. Learn about some of them here.
- See Food: a Guide for People with Alpha-gal Syndrome to learn more about safe and unsafe foods.
Drugs and Medical Products: Established Risks
The medications and other medical products with known risks to people with AGS are listed below.
- Seek the advice of your physician before starting or discontinuing medications and other medical products.
- Experts recommend everyone with AGS avoid some of these medications and medical products (57)(6).
- Others are tolerated by some people with AGS but should be used with caution (57)(6).
- If you are using any of these medical products, seek your physician’s advice about the risks and benefits of switching to alpha-gal-free alternatives.
- If your physician recommends you switch to an alpha-gal-free alternative, but one is not available, consider having your medication compounded by a compounding pharmacy.
- A compounded drug is custom-made by a pharmacy, especially for you.
- A compounding pharmacy is a pharmacy that makes compounded drugs based on individuals’ specific needs.
- Your healthcare provider should be able to recommend a compounding pharmacy.
- Heads up: compounded drugs can be expensive and aren’t always covered by insurance.
- Please refer to Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients by Scott P. Commins and Diagnosis and Management of Patients with the a-Gal Syndrome by Thomas A.E. Platts-Mills et al. for more information.
Drugs and Medical Products: Incomplete Data
- Experts do not routinely recommend against the use of many of the medications and medical products on the “incomplete data” list (57)(6), but be aware that severe reactions to some products on this list by people with AGS have been documented. Therefore, seek your physician’s advice about the use of these products.
- If your physician approves continued use of medications, supplements, and medical products of uncertain risk, take note of any symptoms you experience when you take them.
- Please refer to Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients by Scott P. Commins and Diagnosis and Management of Patients with the a-Gal Syndrome by Thomas A.E. Platts-Mills et al. for more information.
Environment
- Be aware of co-factors, such as exercise, alcohol, non-steroidal anti-inflammatory drugs (like Advil), illness, infection, stress, lack of sleep, and menstruation. These can make your reactions more severe. Exercise and alcohol are especially likely to have an impact (57)(6).
- Be aware that additional tick bites can make your reactions more severe (57)(6). Bee, wasp, and hornet stings can also increase your alpha-gal IgE levels (57) and may lead to more severe reactions, although this hasn’t been established yet.
- Be cautious around airborne alpha-gal, especially fumes from cooking meat, until you know whether you are fume reactive.
- Take note of any reactions to pet saliva or dander.
- In general, more people are bothered by their pet’s saliva than their dander.
- If your pets cause reactions, there are steps you can take to try to keep these under control (see below).
- Fortunately, the vast majority of people with AGS do NOT need to remove pets from their homes (57).
- Watch out for occupational exposures, especially if you work with animals or animal products, such as on a farm, in a restaurant, or in an animal shelter (see below).
- Hobbies like hunting and horseback riding that bring you into contact with mammals, mammalian waste, fluids, and carcasses can also involve risks.
Monitor symptoms
- Take note of any symptoms that persist after you take the above actions.
- Remember to take note of atypical symptoms.
- Remember that different exposures can trigger different symptoms, as described above.
Resources for Step #1
Resources for step #1
Click on the “+” icon to open
Mammalian meat, organs, tissues, and blood
Everyone with alpha-gal syndrome should avoid most of the foods on this list (6,57). You may have had mild reactions after eating red meat, but a future reaction could be more serious, as explained above. Up to 60% of people with AGS have anaphylactic reactions (24,78,87,88,89), and 30-40% have cardiac and respiratory symptoms (90). Don’t play Russian roulette!
- Mammalian meats (1,6,57), such as beef, pork, lamb, bison, venison, goat, horse, rabbit, squirrel, kangaroo, antelope, buffalo, camel, guinea pig, bats, whales, etc.
- If you aren’t sure which animals are mammals, there is a guide here.
- The internal organs of mammals, like liver (21), lung, heart, intestines (tripe or offal), and kidneys (6,57).
- Mammalian gut sausage casings (6,57).
- Mammalian fat, like lard, tallow, and suet*
- Mammalian fat is often in cooked foods, such as sauces, pastries, pie crusts, tortillas, tortilla chips, refried beans, baked beans, vegetable dishes, mashed potatoes, and desserts.
- Some baking mixes (like Jiffy Corn Muffin Mix) contain lard.
- Beef fat is often added to fry oil to enhance flavor (6,57).
- Bones and bone marrow
- Testicles (Rocky Mountain or prairie oysters)
- Mammalian skin (like pork rinds and ponmo)
- Mammalian collagen (e.g., beef collagen sausage casings) (6,57)*
- Meat broth, bouillon, and stock (6,57)**
- Gravy (6,57)
- Mammalian blood, found in soups, black pudding, blood sausage, blodplättar, and other foods
- Meat broths, bouillon, stocks, and gravy (6,57)**
- Meat extracts, like Bonox and Bovril***
- All other mammalian body parts, organs, tissues, cells, and fluids, such as tendons, brain, lungs, heart, nerves, skin, mammalian bile (Papait seasoning), and the products that contain them.
*”Some subjects can tolerate without allergic reactions but should be used with caution” (6)
**”Stocks and bouillon cubes: these are often derived from mammalian sources and additional research is needed to understand the risks from these and other hidden exposures.” (57)
***We aren’t aware of any published information about the risks of these products, but caution seems advisable.
Some experts may advocate less restrictive guidelines for some asterisked foods for their least reactive patients (57)(6). Still, as many people with AGS report that some of their worst reactions occurred after eating them (especially lard), we recommend that most people avoid them completely, unless their physician advises otherwise.
See Food: A Guide for People with Alpha-gal Syndrome for more information.
Flounder roe (flounder eggs)
Japanese studies found that people with AGS can have severe reactions after eating the roe (eggs) of some flounder species (26, 104). There is no evidence of alpha-gal in most other fish eggs, including the non-flounder fish roes most commonly eaten in the U.S., but proceed with caution when trying new and exotic types of fish roe.
Medications, medical devices, other medical products, and supplements
We have done our best to find and compile available information from disparate sources and update it when we can. Still, data on the risks of alpha-gal in medical products is incomplete, and there is no comprehensive source of information about all alpha-gal-containing medical products and the risks they pose. Therefore, this is not a complete list. Please consult a physician for more information.
Established risk*
There is clear evidence that these medications and medical products contain alpha-gal, AND:
- Commins (57) and/or Platts-Mills et al. (6) have identified them as either best avoided by everyone with alpha-gal syndrome or used only with caution OR
- Kuravi et al. have suggested that they “may lead to adverse reactions clinically” based on their alpha-gal content (103).
Some people with AGS can tolerate some of these products. Please refer to Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients and Diagnosis and Management of Patients with the α-Gal Syndrome and/or consult an expert for more information.
- Cetuximab (a drug that played a role in the discovery of AGS) (6,30,31,57)
- Gelatin-based plasma volume expanders, such as Gelafundin, Gelofusine, Gelaspan, Haemaccel (not commonly used in the U.S. if at all) (6,28,52,57,101). Even some people who are not reactive to mammalian meat react to these products (28). Platts-Mills, et al. recommend avoidance for everyone with active AGS (6).
- Many vaccines, including those that contain gelatin or other mammalian byproducts. Gelatin appears to be the most problematic vaccine excipient for people with AGS.
- In the U.S., vaccines that contain gelatin include (but are not necessarily limited to): Zostavax, MMR, yellow fever, rabies, oral typhoid, FluMist, Boostrix, and others (6,28,39,42,43,57,92).
- There is incomplete, if any, data on risks associated with vaccines containing other potential sources of alpha-gal, such as vaccines produced in mammalian lines like Madin-Darby Canine Kidney cells (e.g., Flucelvax). Therefore, experts may recommend alternatives to these vaccines when they are available (114).
- Use the CDC Pink Book database (below) and contact manufacturers for information about vaccine ingredients.
- When your physician feels the benefits of an alpha-gal-containing vaccine outweigh the potential risks, consult an allergist about graded dosing and other safety protocols.
- Heparin: Dr. Scott Commins reports: “Importantly, we have not had issues with routine heparin prophylaxis for deep venous thrombosis (DVT) and our experience suggests this can be safely administered for the overwhelming majority of patients with AGS. There are, undoubtedly, exceptions that will require alternate forms of DVT prophylaxis. Heparin-based reactions that are much more common include those clinical scenarios where heparin is given at high doses for more complete anti-coagulation, such as during heart catheterization, valve procedures, and extracorporeal membrane oxygenation (ECMO).” (57).
- Bioprosthetic (bovine and porcine) heart valves (6,45,46,47,48,49,57,103) including:
- Pancreatic enzyme replacements, such as pancrelipase and other enzyme replacements (e.g., Viokase, Pertzye, Zenpep (Allergan), Creon)(6,36,57, 103) and Pancreatin (Now Foods, Bloomingdale, Ill)– an over-the-counter dietary aid (103).
- These are produced from the pancreas of non-primate mammals and can contain high levels of alpha-gal.
- Antivenom, such as crotalidae polyvalent immune Fab (CroFab) (6,50,51,57)
- Many thyroid hormones replacements, including Armour Thyroid (Allergan) (57,103)
- We are not aware of any published, expert advice on the use of these products by people with AGS. Still, Kuravi et al. demonstrated high alpha-gal content and the products’ ability to bind patient IgE and commented that it “may lead to adverse reactions clinically” (103).
- Heart patches, including CorMatrix Cor™ PATCH– an epicardial patch for cardiac tissue repair (103)
- Collagen scaffolding, including Cardiocel acellular collagen scaffold (LeMaitre Vascular, Burlington, Mass)– used in heart and vascular repair (103)
- Photofix (decellularized bovine pericardium (Cryolife, Kennesaw, Ga)– used in heart and vascular repair (103)
- ProCol bovine mesenteric vein (LeMaitre Vascular) (103)
- EnteraGam (Entera Health, Cary, NC), a bovine immunoglobulin and immunoprotein isolate for the management of irritable bowel syndrome and inflammatory bowel disease (103).
Incomplete data
There is limited evidence that these products contain alpha-gal and/or contribute to clinical reactions in people with alpha-gal syndrome (57)(6); however, there are published and unpublished accounts of patients with alpha-gal syndrome having severe reactions to some of them. Please refer to Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients and Diagnosis and Management of Patients with the α-Gal Syndrome and/or consult an expert for more information.
- Hemostatic agents, such as
- Other products that contain gelatin, such as:
- In general, parenterally administered gelatin-containing products are considered riskier than orally administered medical products.
- Find more information about gelatin in medical products and the risks associated with them here.
- Monoclonal antibodies (other than cetuximab): many monoclonal antibodies (mAbs) are produced in non-primate mammalian cell lines, but evidence for alpha-gal expression on most, other than cetuximab, is minimal (57)(6).
- Many other perioperative, prescription, and OTC drugs (6,32,33,34,35,57). Some of these pose a known risk to people with AGS; others contain mammalian byproducts for which there is little data on alpha-gal content or their ability to contribute to clinical reactions. These drugs include:
- Stearic acid
- Magnesium stearate (38) (in many tablets)
- Glycerin (in many suspensions)
- Lactose and lactose derivatives
- Dairy byproducts in drugs and vaccines including (but not limited to), casamino acids, casein, and lactalbumin.
- Lactose alone is used in more than 20% of prescription drugs and about 6% in over-the-counter medicines.
- Many other medical products and devices, including (but not limited to) catgut and collagen sutures, lubricants, topicals, adhesives (including bandage adhesives), extracellular matrix (ECM) scaffolds, etc. (6,32, 33, 34, 35, 102)
*Established risk: categorized as primary or secondary risk by Platts-Mills, et al (6), listed as a relevant medical exposure by Commins (57), or described by Kuravi et al as “may lead to adverse reactions clinically” (103).
Airborne exposures
There are no published data on the percentage of people with alpha-gal syndrome (AGS) who react after exposure to airborne alpha-gal, but the informal estimates of experts range from 10-30% (113, 114). People with AGS who react to airborne alpha-gal report that reactions often start within minutes of exposure, progress quickly, and can be severe.
- Suspended fat droplets and aerosols in smoke or fumes from cooking meat, especially from grills, barbeques, and sometimes frying meat, are by far the most commonly reported airborne trigger of alpha-gal reactions (57).
- Until you know whether you react to airborne alpha-gal, exercise caution around possible sources of exposure, especially barbecues and other types of cooking that generate aerosolized mammalian fat.
- If you experience dizziness, breathing difficulty, or other symptoms, remove yourself immediately from the source of exposure!
- Some people with AGS report that fume reactions are the most dangerous reactions that they experience, leading rapidly to anaphylaxis, airway issues, and/or unconsciousness.
For more information about reactions to airborne alpha-gal, including reported symptoms other sources of airborne alpha-gal that may trigger reactions, see Reactions to Airborne Alpha-gal: A Guide for People with Alpha-gal Syndrome.
Pets
If you suspect that your pet may be triggering alpha-gal reactions, try the following:
- Stop sleeping with your pet. Instead, move your pet’s bed out of the bedroom. This is important for tick avoidance as well.
- Don’t let your pet lick you. Pet saliva causes more people to react than pet dander.
- If your pet does lick you, wash with soap and water right away.
- Pet dander can trigger airborne reactions. Take note of any airborne reactions to pet dander.
- If pet dander bothers you, wash them more frequently and consider buying a HEPA to put next to your pet’s sleeping area.
- If you continue to react after contact with your pet, try washing your hands after you pet them.
- Switch your pet’s food to a brand that contains fish or chicken, instead of mammal. Many people find that this helps the most.
- Switch to vegan grooming supplies.
- Unfortunately, some people find that they need to find new homes for their pets after they develop AGS, but this is uncommon.
Farm animals and hunting
Hunters, farmers, butchers, and slaughterhouse workers need to be alert to the possibility of reactions from occupational exposures including:
- Animal waste and fumes from animal waste
- Amniotic fluid during calving
- Exposure to blood, meat, and other tissue during the processing of carcasses
- Contact with mammalian saliva or other mammalian fluids
- Other contacts
Food

Food: First Steps
Foods to avoid, substitutes for red meat products and other tips.

What Is a Mammal?
Which animals are mammals? Which aren’t?

Amaroo Hills Emu Farm
Emu and ostrich steaks, ground emu, breakfast and Italian sausage, emu pastrami and more. Tastes just like the red meat you love!

Fossil Farms
Fossil farms sells ostrich, emu, guinea fowl, pheasants, quail, and squab, etc.
Drugs and Medical Products
DailyMed
The National Library of Medicine (NLM)’s DailyMed searchable database provides information for prescription and nonprescription drugs and other medical products.
Search by the NDC# of a drug or other medical product to find its ingredients, including inactive ingredients.

Robert Wood Johnson Hospital Drug Information Center
Hours: M-F 8:30am-4:30pm
Email: njdruginfo@rwjbh.org
Phone: (732) 937-8842
The RWJ Drug Information Center can help you & your providers determine whether drugs and other medical products contain alpha-gal. You will need to provide the NDC# of the products.

CDC: Pink Book Vaccine Excipient Summary
Information about excipients in vaccines available in the U.S.
Drugs Compounding

Info on Drug Compounding from the FDA
Drug compounding is often regarded as the process of combining, mixing, or altering ingredients to create a medication tailored to the needs of an individual patient.

What Are Compounding Pharmacies?
Information from GoodRX Health

Find a Compounding Pharmacy Near You
Step #2
For people whose symptoms are not controlled by Step #1
Reactivity to gelatin is not uncommon among patients with AGS; however most patients tolerate the smaller exposures of everyday life (57).
Although carrageenan is known to contain alpha-gal epitopes, clinical experience suggests the risk of reactions appears to be quite low and is likely pertinent to 1-2% of patients (57).
Carrageenan causes a more immediate reaction than typical for me. It causes abdominal bloating and GI issues lasting at least two days. I become very fatigued, my body becomes flushed, I get hives, and get foggy in the mind. It’s one of the worst reactions I’ve had and it’s in vegan sour cream and ice cream!
Some people take all actions in Step #1 but still have symptoms. Sometimes these aren’t the same symptoms that eating meat triggers. Instead, they may be atypical allergic symptoms like GI issues, muscle pain, joint pain, or headaches. If this happens to you, you may want to try the following:
Food
- Eliminate moderate risk foods, such as those that contain rennet, dairy, gelatin, and carrageenan
- Some people begin avoiding these all at once; some try giving up one category at a time, often in the order below. However, as everyone’s reactions are different, this might not be the right order for you. For example, some people react more to gelatin than to dairy.
- Cheeses and other dairy made with rennet
- Other high-fat dairy products, like butter and ice cream
- Lower fat dairy products
- Gelatin
- Carrageenan
- Natural flavors and flavorings, which are often derived from beef or pork, especially in savory foods (57)
- Watch out for cross-contamination at home and when eating out.
- Make sure your poultry hasn’t been injected with mammalian broths, carrageenan, or “natural flavorings.”
- Fish and other seafood may be treated with processing agents, such as carrageenan. Try to buy direct, so you know who, how, where, and when your seafood was caught, processed, and distributed. Ask if seafood is treated. Seafood flash-frozen immediately after it is harvested is less likely to be contaminated. Some people in the AGS community buy from Wild Alaskan Company, which claims that nothing but water is used on their seafood.
- For unknown reasons, some people react to canned tuna (6). This may be due to the use of carrageenan or other processing agents. However, some of us have had good luck with Wild Planet pole caught tuna.
Drugs, Medical Products, and Supplements
- Avoid gummy supplements.
- Talk to your healthcare provider and pharmacist about gelatin-free alternatives to medications in gelatin capsules and other gelatin-containing drugs. Tablets and liquid forms of medication are often gelatin-free, but watch out for carrageenan in liquids.
- Most vitamin D3 is derived from sheep’s wool.
- If you are taking daily vitamin D3 supplements, this may contribute to your reactions.
- Switch to vegan vitamin D3, which is derived from lichens.
- Watch out for vitamin D3 added to foods and drinks, especially milk (if you still drink it), cereal, and orange juice.
- Pure Encapsulations is one recommended source of supplements.
- Their formulations are simple and designed to be hypoallergenic.
- Not all their products are alpha-gal-free. Use the search function to search for their vegan products.
- You can’t buy directly from Pure Encapsulations.
- Pure Formulas is one of their authorized suppliers.
- Take note of any reactions to the following:
- Medications and supplements containing mammalian byproducts, like lactose or magnesium stearate
- Drugs and medical products containing carrageenan
- Drugs and medical products containing lanolin, which is derived from sheep’s wool.
- For example, many topical ointments contain lanolin.
Environment
- If you are fume sensitive, avoid airborne alpha-gal, especially fumes from cooking meat, and explore other options for managing reactions to airborne alpha-gal here.
- See tips below if you react to your pets’ dander or saliva.
- If you work with animals, keep livestock at home, or hunt, be aware of associated exposures that can lead to reactions, such as exposure to mammalian blood, waste, and amniotic fluid.
- Take note of reactions to personal care products containing gelatin and lanolin.
- Take note of reactions to wool.
- Reactions to leather can also occur.
- Consider switching to a vegan toothpaste that does not contain carrageenan.
- If you think you may be reacting to personal care products, see Personal Care Products: a Guide for People Highly Sensitive to Alpha-gal.
- If you think household products may be triggering reactions, see Step #3 (coming soon) for more information.
Monitor symptoms
- Take note of any symptoms that persist after you take the above actions.
- If your symptoms are still not under control after taking the above actions, move to Step #3.
Resources for Step #2
Resources for step #2
Click on the “+” icon to open
Rennet
Rennet is a complex set of enzymes sometimes used in foods, especially cheese. Most rennet is extracted from the stomachs of ruminant mammals, although sometimes vegetable and microbial rennets are used. It’s not uncommon for people who tolerate other types of dairy to react to cheese made with rennet.
Rennet may also be listed on labels as:
- Enzymes
- Traditional rennet
- Rennin (also called chymosin)
Products that contain rennet include:
- Parmesan
- Some other cheeses, especially hard cheeses
- Packaged macaroni and cheese
- Desserts, like Junket
Tips:
- Look for cheeses labeled “vegetarian.”
- Find cheeses that don’t contain rennet on the Vegetatio list of vegetarian cheeses.
- Read Bad News: These 11 Cheeses Aren’t Always Vegetarian for a list of some, but not all, cheeses that do contain rennet.
- See The Definitive Guide to Vegetarian Cheese for more info about cheese made with and without rennet.
- Is Cheese Vegetarian? is a quick guide to finding information about rennet on cheese labels.
Lipase is another mammalian byproduct used in cheesemaking. There is insufficient data to determine whether it contains alpha-gal or whether people with AGS react to it, but it is derived from porcine pancreas, which has high alpha-gal content.
Milk and dairy products
10-33% (57,85) of people with AGS react to milk and dairy products.
- As alpha-gal is believed to be concentrated in animal fat, high-fat dairy products like ice cream and butter are the most likely to trigger reactions (57).
- Some people can tolerate cheese that is not made with rennet, especially low-fat cheeses.
- Cream contains more alpha-gal than milk, but many people who react to higher-fat dairy products tolerate both.
- See the Wikipedia list of dairy products to see which other foods are dairy products.
Some people who don’t tolerate dairy products also react to dairy byproducts in foods, drugs, and other products:
- Whey protein powder, a concentrated form of milk protein, can trigger reactions even in people who tolerate other dairy products. Look for it in protein powders, protein bars, and supplements (29). Anecdotal reports suggest that whey is one of the more problematic dairy byproducts for people with AGS.
- Casein is another common dairy byproduct. It’s not clear whether casein is glycosylated with alpha-gal or not, but caution is recommended for dairy-sensitive members of the alpha-gal community.
- There are several lists of dairy products and dairy byproducts. GoDairyFree’s Dairy Ingredient List and Milk Allergy Avoidance List are among the most helpful.
- For a wallet-sized card with some of the more common dairy byproducts, see Kelly Mom’s Hidden Dairy “Cheat Sheet.”
- Dairy byproducts in drugs and vaccines include (but are not limited to) lactose, casamino acids, casein, and lactalbumin. Lactose alone is used in more than 20% of prescription drugs and about 6% in over-the-counter medicines. However, most drugs that contain dairy byproducts do not bother most people with AGS.
Shopping tips:
- Check labels. Milk is a Big 8 allergen and must be declared on ingredient lists of many, but not all, foods and drinks. Foods and beverages that do NOT have to be labeled include meat, fish, egg products, fresh fruits and vegetables, and alcoholic beverages.
- Medications, supplements, personal care and household products are also not required to have dairy ingredients declared on their labels.
- Learn the difference between “non-dairy” vs “dairy-free.”
- Beware of dairy byproducts in non-dairy products, including whey and casein.
- If you react to dairy byproducts, stick to “dairy-free” products but remember to check them for mammalian byproducts that are not from milk, like vitamin D3 (from lanolin) and carrageenan.
GoDairyFree is a great website with much more information about dairy allergies and helpful reviews of dairy-free products.
Gelatin
Fewer than 10% of people with AGS react to gelatin in foods (57), but some have severe reactions (27,28). Gelatin can be consumed through the mouth (for example when we eat gelatin in foods or swallow medications in gelatin capsules) or administered some other way, as with vaccines and medications delivered through an IV. In this section we ONLY deal with gelatin in foods. People who tolerate gelatin in foods, supplements, and some medications, may experience severe and sudden-onset symptoms, including anaphylaxis, when medical products containing gelatin are injected or administered through an IV (6,28,52,57). There have also been cases of gelatin in vaginal capsules triggering anaphylaxis (37).
- Gelatin is made from collagen derived from the bones, skin, and other parts of animals.
- Most gelatin is from cows or pigs and contains alpha-gal. Some products are made with fish gelatin, which is safe for people with AGS, but these are rare.
- Fewer of us react to gelatin in foods than to dairy, but for some of us, our reactions to gelatin are worse than our dairy reactions.
- Gelatin can also be listed on labels as hydrolyzed animal protein, collagen hydrolysate, denatured collagen, and gelatina. Other names for gelatin, including trade names, are listed here and here.
- Gelatin is used as an ingredient in many foods as a stablizer, thickener, texturizer and to improve the mouth-feel of reduced-fat foods.
- Gelatin is also used as a processing aid, for example to clarify beverages, like wine, beer and juice. Processing aids do not need to be listed as an ingredient.
- Foods that can contain gelatin include, but are not limited to:
- Candy including Starburst, Altoids, gummy worms and other gummy candies, peeps, some candy corn, and jelly beans
- Gummy vitamins and supplements, including fish oil in gelatin capsules
- Jello gelatin
- Marshmallows
- Dairy products, including yogurt, ice cream, whipped cream, sour cream, cream cheese, cottage cheese, cheese spreads, and semi-fat cheese spreads
- Margarine
- Desserts, including popsicles, instant dessert powders, cakes or cake fillings, instant puddings, cheesecake
- Jellies and jams
- Icing and frosting
- Syrups
- Snacks, including Rice Krispy Treats, Poptarts, snack bars, and fruit-flavored snacks
- Pastries and other baked goods
- Some cereals, like Lucky Charms, Kellogg’s Frosted Mini-Wheats and other frosted cereals, cereals with marshmallows in them, and many others.
- Peanuts, such as Planters Dry Roasted Peanuts, which are coated with gelatin to help the salt stick
- Fruit salads
- Food foams (espuma)
- Aspic
- Dips
- Soups and stock, including jellied tomato consommé
- Sauces
- Glazes
- Meats and meat products, including:
- Bouillon
- Sausage coatings
- Ground meat
- Sausages
- Frozen turkey products
- Lunch meats
- Chicken rolls
- Canned meat
- Turkey
- Instant gravy, instant sauces and soups
- Beverages, including:
- Animal glue, for example, as an adhesive on stickers used on fruit
- As a coating on fresh vegetables and fruit
- Gelatin is used as a processing aid for:
- Clarification of beverages such as wine, beer, vegetable and fruit juice (especially apple juice), and possibly vinegar
- Microencapsulation of colors, flavors, oils, vitamins
It’s important to remember that it’s not just food that can contain gelatin.
- Many medications and supplements contain gelatin, especially those in capsules. For most medications, there are alternatives that do not contain mammalian-derived ingredients like gelatin. In cases where there aren’t alternatives, you may need to way the risks of exposure to gelatin–which vary from individual to individual and product to product–against the benefits of taking the a medication. Seek your doctor’s advice about what to do if your supplements or medications contain gelatin.
- Many personal care products contain gelatin.
If you react to gelatin, remember to always check labels to see if foods, medications, and personal care products contain it before you buy them. Fish gelatin is not from mammals and many people with AGS use it as a substitute for mammalian gelatin.
See Gelatin: A Guide for People with Alpha-gal Syndrome for more information.
Carrageenan
At least 1-2% of people with AGS report reacting to carrageenan (57)(6). Many of us think the actual number is much higher and that the small number reported in the literature is due to patients failing to connect their reactions to carrageenan and reporting them as dairy-related. For example, multiple reports of reactions to the Dairy Queen blizzard have been attributed to the blizzard’s dairy content, but blizzards also contain carrageenan.
- Carrageenans are a family of linear sulfated polysaccharides extracted from red edible seaweeds. They are widely used in the food industry for their gelling, thickening, and stabilizing properties.
- Although carrageenans are not derived from mammals, they contain the alpha-gal epitope (54).
- There isn’t much in the literature about carrageenan reactions in people with AGS, but many of us react to carrageenans, and our reactions can be severe.
- Carrageenans are widely used in the food industry as:
- Ingredients, for their gelling, thickening, and stabilizing properties
- Processing agents used in the clarification of beer and juice
- Coating materials sprayed on cut organic fruit
- Water retention agents applied to fish before processing
- Functional agents in the production of cheese
- Clarifiers and heat stabilizers in wine
- Other foods that can contain carrageenan include, but are not limited to:
- Many dairy products, including ice cream; milkshakes, like Dairy Queen blizzards; yogurt; flavored, evaporated, and condensed milk; whipped topping; cheeses; and sour cream (76)
- Many dairy-free substitutes (57)
- Desserts, including flans, custards, cream puddings, mousse, sorbet, gelato, and gel desserts (76,77)
- Drink mixes (powdered lemonade, fruit punch) (77)
- Juices, ready to spread icings, jams, jellies, salad dressing, and candies (76,77)
- Salad dressing, mayonnaise, and relishes (77)
- Poultry products: raw poultry is often injected with carrageenan and it is frequently added to deli meats and other processed poultry products to enhance texture (77)
- Drinks, such as beer and juice clarified by carrageenan (77)
- Seafood, such as fish treated with carrageenan to improve moisture retention (77)
- Tofu (77)
- Infant formula (77)
Carrageenan is also in some personal care products, like toothpaste, and medical products.
As with gelatin, it is possible that carrageenan in some medical products may have a greater potential to cause serious reactions than carrageenan in foods, but there is no published or unpublished data on this, as far as we are aware.
See Carrageenan: A Guide for People with Alpha-gal Syndrome for more information.
Cross-contamination (cross-contact)
An unknown percentage of people with AGS react to food contaminated by mammalian meat or other mammalian products, including some people who tolerate dairy and other moderate risk foods. A contributing factor to the risk posed by cross-contamination (also called cross-contact) is the heat stability of alpha-gal which, unlike protein allergens, is not denatured at normal cooking temperatures. Another issue is that fat seems to be the primary antigenic form of alpha-gal. Fat is less likely to be removed from grills, pots, pans, and other surfaces during cleaning than proteins. Also, droplets of fat from cooking meat can contaminate nearby food.
Some of the more common sources of alpha-gal contamination include:
- Grills, pots, pans, spatulas, and other cooking utensils.
- Cooking utensils used to for mammalian meats and other products need to be thoroughly cleaned after use.
- Grills are a common problem, and many people with AGS buy a separate grill for cooking alpha-gal-free foods.
- In restaurants, avoid grilled foods unless they are cooked on a separate grill from the any used for cooking mammalian meat.
- Droplets of fat from splatter or fumes from cooking meat
- Contaminated cutting and preparation surfaces
- Contaminated knifes and other kitchen cutlery, when not cleaned between uses
- Sponges used to clean items contaminated with meat fat.
- Wooden, plastic and heavily-scratched cooking utensils can trap fat even when cleaned, as can cast-iron pans, if they aren’t scrubbed and re-seasoned.
- Improper storage of food in refrigerators: store mammalian meat on the bottom shelf or in a separate refrigerator drawer.
- Ovens and microwaves contaminated with mammalian grease
Additional sources of contamination markets, restaurants, and manufacturing facilities:
- Fry oil: sometimes animal fat is added to fry oil for flavor, but even when it’s not, oil can be contaminated if mammalian meats or products were fried in it previously.
- Grinders and sausage making equipment: ground poultry and poultry sausages are frequently contaminated with other meats when contaminated grinders and other equipment are used.
- Deli meat slicers: sliced turkey and cheese (for those who tolerate it) can be contaminated when sliced on with contaminated slicers.
- Butchers and meat departments: cross-contamination can occur during handling
- Gloves, if not changed after handling mammalian products
- Shared processing lines/facilities.
See Cross-Contamination: A Guide for People with Alpha-gal Syndrome for more information.
Gelatin and Carrageenan

Gelatin
A Guide for People with Alpha-gal Syndrome
Carrageenan
A Guide for People with Alpha-gal Syndrome
Food: Dairy

Go Dairy Free
Information on the dairy-free diet: dairy-free recipes, product reviews, news, recommend-ations and health guides.
Kelly Mom Hidden Dairy Cheat Sheet
Wallet card
Food: Other

Cross-contamination
A Guide for People with Alpha-gal Syndrome

The AlphaGal Kitchen Facebook Group
A place for those that are mastering their alpha gal allergy to share their alpha gal kitchen recipes and experiences.

Seafood Finder
Use this tool from Local Catch to find local fishers and seafood harvesters who sell directly to consumers.

Wild Alaska Seafood Company
A monthly seafood membership that delivers sustainably-sourced seafood to your doorstep.
Supplements

Pure Encapsulations
Supplements formulated without unnecessary additives and many common allergens. Not all are alpha-gal-free. Use the search function to search for vegan products. One authorized dealer is Pure Formulas.

NIH Dietary Supplement Label Database
Search over 130,000 labels in the Dietary Supplement Label Database.
Still reacting? Next Steps
If you have completed Steps #1 and #2 and are still having reactions, you may be highly sensitive to alpha-gal. Find more information for people highly sensitive to alpha-gal at the links below.

Determining Your Tolerance to Alpha-gal: Next Steps
A guide for people highly reactive to alpha-gal.
COMING SOON!

Personal Care Products
A guide for people highly reactive to alpha-gal.

Household Products
A guide for people highly reactive to alpha-gal.
COMING SOON!
References
1. Commins SP, Satinover SM, Hosen J, Mozena J, Borish L, Lewis BD, Woodfolk JA, Platts-Mills TA. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-α-1, 3-galactose. Journal of Allergy and Clinical Immunology. 2009 Feb 1;123(2):426-33.
2. Commins S, Lucas S, Hosen J, Satinover SM, Borish L, Platts-Mills TA. Anaphylaxis and IgE antibodies to galactose-alpha-1, 3-galactose (alphaGal): insight from the identification of novel IgE ab to carbohydrates on mammalian proteins. Journal of Allergy and Clinical Immunology. 2008 Feb 1;121(2):S25.
3. Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, Kocan KM, Fahy JV, Nganga LW, Ronmark E, Cooper PJ. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1, 3-galactose. Journal of Allergy and Clinical Immunology. 2011 May 1;127(5):1286-93.
4. Soh JY, Huang CH, Lee BW. Carbohydrates as food allergens. Asia Pacific Allergy. 2015 Jan 1;5(1):17-24.
5. Levin M, Apostolovic D, Biedermann T, Commins SP, Iweala OI, Platts-Mills TA, Savi E, van Hage M, Wilson JM. Galactose α-1, 3-galactose phenotypes: Lessons from various patient populations. Annals of Allergy, Asthma & Immunology. 2019 Jun 1;122(6):598-602.
6. Platts-Mills TA, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-Gal syndrome. The Journal of Allergy and Clinical Immunology: In Practice. 2020 Jan 1;8(1):15-23.
7. Commins SP. Invited commentary: alpha-gal allergy: tip of the iceberg to a pivotal immune response. Current allergy and asthma reports. 2016 Sep 1;16(9):61.
8. Crispell G, Commins SP, Archer-Hartman SA, Choudhary S, Dharmarajan G, Azadi P, Karim S. Discovery of alpha-gal-containing antigens in North American tick species believed to induce red meat allergy. Frontiers in immunology. 2019 May 17;10:1056.
9. Monzón JD, Atkinson EG, Henn BM, Benach JL. Population and evolutionary genomics of Amblyomma americanum, an expanding arthropod disease vector. Genome biology and evolution. 2016 May 1;8(5):1351-60.
10. Raghavan RK, Peterson AT, Cobos ME, Ganta R, Foley D. Current and future distribution of the lone star tick, Amblyomma americanum (L.)(Acari: Ixodidae) in North America. PLoS One. 2019 Jan 2;14(1):e0209082.
11. Wilson JM, Platts-Mills TA. Red meat allergy in children and adults. Current opinion in allergy and clinical immunology. 2019 Jun 1;19(3):229-35.
12. Commins, SP. (2018). Retrieved from: More people developing red meat allergy from tick bites. CBS News
13. Flaherty MG, Threats M, Kaplan SJ. Patients’ Health Information Practices and Perceptions of Provider Knowledge in the Case of the Newly Discovered Alpha-gal Food Allergy. Journal of Patient Experience. 2020 Feb;7(1):132-9.
14. Flaherty MG, Kaplan SJ, Jerath MR. Diagnosis of life-threatening alpha-gal food allergy appears to be patient driven. Journal of primary care & community health. 2017 Oct;8(4):345-8.
15. Cabezas-Cruz A, Hodžić A, Román-Carrasco P, Mateos-Hernández L, Duscher GG, Sinha DK, Hemmer W, Swoboda I, Estrada-Peña A, De La Fuente J. Environmental and molecular drivers of the α-Gal syndrome. Frontiers in Immunology. 2019 May 31;10:1210.
16. Commins SP, Platts-Mills TA. Tick bites and red meat allergy. Current opinion in allergy and clinical immunology. 2013 Aug;13(4):354.
17. Stoltz LP, Cristiano LM, Dowling AP, Wilson JM, Platts-Mills TA, Traister RS. Could chiggers be contributing to the prevalence of galactose-alpha-1, 3-galactose sensitization and mammalian meat allergy?. The journal of allergy and clinical immunology. In practice. 2019 Feb;7(2):664.
18. Arkestål K, Sibanda E, Thors C, Troye-Blomberg M, Mduluza T, Valenta R, Grönlund H, van Hage M. Impaired allergy diagnostics among parasite-infected patients caused by IgE antibodies to the carbohydrate epitope galactose-α1, 3-galactose. Journal of Allergy and Clinical Immunology. 2011 Apr 1;127(4):1024-8.
19. Chinuki Y, Ishiwata K, Yamaji K, Takahashi H, Morita E. Haemaphysalis longicornis tick bites are a possible cause of red meat allergy in Japan. Allergy. 2016 Mar;71(3):421-5.
20. Hashizume H, Fujiyama T, Umayahara T, Kageyama R, Walls AF, Satoh T. Repeated Amblyomma testudinarium tick bites are associated with increased galactose-α-1, 3-galactose carbohydrate IgE antibody levels: a retrospective cohort study in a single institution. Journal of the American Academy of Dermatology. 2018 Jun 1;78(6):1135-41.
21. Bianchi, John (2019). Personal communication
22. Morisset M, Richard C, Astier C, Jacquenet S, Croizier A, Beaudouin E, Cordebar V, Morel‐Codreanu F, Petit N, Moneret‐Vautrin DA, Kanny G. Anaphylaxis to pork kidney is related to IgE antibodies specific for galactose‐alpha‐1, 3‐galactose. Allergy. 2012 May;67(5):699-704.
23. Fischer J, Hebsaker J, Caponetto P, Platts-Mills TA, Biedermann T. Galactose-alpha-1, 3-galactose sensitization is a prerequisite for pork-kidney allergy and cofactor-related mammalian meat anaphylaxis. Journal of allergy and clinical immunology. 2014 Sep 1;134(3):755-9.
24. Fischer J, Yazdi AS, Biedermann T. Clinical spectrum of α-Gal syndrome: from immediate-type to delayed immediate-type reactions to mammalian innards and meat. Allergo journal international. 2016 Mar 1;25(2):55-62.
25. McPherson TB, Liang H, Record RD, Badylak SF. Galα (1, 3) Gal epitope in porcine small intestinal submucosa. Tissue engineering. 2000 Jun 1;6(3):233-9.
26. Fujiwara M, Araki T. Immediate anaphylaxis due to beef intestine following tick bites. Allergology International. 2019;68(1):127-9.
27. Caponetto P, Fischer J, Biedermann T. Gelatin-containing sweets can elicit anaphylaxis in a patient with sensitization to galactose-α-1, 3-galactose. The Journal of Allergy and Clinical Immunology: In Practice. 2013 May 1;1(3):302-3.
28. Mullins RJ, James H, Platts-Mills TA, Commins S. Relationship between red meat allergy and sensitization to gelatin and galactose-α-1, 3-galactose. Journal of Allergy and Clinical Immunology. 2012 May 1;129(5):1334-42.
29. Kaman K, Robertson D. ALPHA-GAL ALLERGY; MORE THAN MEAT?. Annals of Allergy, Asthma & Immunology. 2018 Nov 1;121(5):S115.
30. Chung CH, Mirakhur B, Chan E, Le QT, Berlin J, Morse M, Murphy BA, Satinover SM, Hosen J, Mauro D, Slebos RJ. Cetuximab-induced anaphylaxis and IgE specific for galactose-α-1, 3-galactose. New England journal of medicine. 2008 Mar 13;358(11):1109-17.
31. Berg EA, Platts-Mills TA, Commins SP. Drug allergens and food—the cetuximab and galactose-α-1, 3-galactose story. Annals of Allergy, Asthma & Immunology. 2014 Feb 1;112(2):97-101.
32. Dunkman WJ, Rycek W, Manning MW. What does a red meat allergy have to do with anesthesia? Perioperative management of alpha-gal syndrome. Anesthesia & Analgesia. 2019 Nov 1;129(5):1242-8.
33. Pfützner W, Brockow K. Perioperative drug reactions–practical recommendations for allergy testing and patient management. Allergo journal international. 2018 Jun 1;27(4):126-9.
34. Dewachter P, Kopac P, Laguna JJ, Mertes PM, Sabato V, Volcheck GW, Cooke PJ. Anaesthetic management of patients with pre-existing allergic conditions: a narrative review. British journal of anaesthesia. 2019 Jul 1;123(1):e65-81.
35. Popescu FD, Cristea OM, IONICĂ FE, Vieru M. DRUG ALLERGIES DUE TO IgE SENSITIZATION TO α-GAL. magnesium. 2018;2017:47-8.
36. Swiontek K, Morisset M, Codreanu-Morel F, Fischer J, Mehlich J, Darsow U, Petitpain N, Biedermann T, Ollert M, Eberlein B, Hilger C. Drugs of porcine origin—A risk for patients with α-gal syndrome?. The Journal of Allergy and Clinical Immunology: In Practice. 2019 May 1;7(5):1687-90.
37. Vidal C, Mendez-Brea P, Lopez-Freire S, Gonzalez-Vidal T. Vaginal Capsules: An Unsuspected Probable Source of Exposure to α-Gal. Journal of investigational allergology & clinical immunology. 2016;26(6):388.
38. Muglia C, Kar I, Gong M, Hermes-DeSantis ER, Monteleone C. Anaphylaxis to medications containing meat byproducts in an alpha-gal sensitized individual. The journal of allergy and clinical immunology. In practice. 2015;3(5):796.
39. Akella K, Patel H, Wai J, Roppelt H, Capone D. Alpha Gal-Induced Anaphylaxis to Herpes Zoster Vaccination. Chest. 2017 Oct 1;152(4):A6.
40. Bakhtiar MF, Leong KW, Kwok FY, Hui MT, Tang MM, Joseph CT, Bathumana‐Appan PP, Nagum AR, ZHM Y, Murad S. P66: ALLERGIC REACTION TO BOVINE GELATIN COLLOID: THE ROLE OF IMMUNOGLOBULIN E TOWARDS GALACTOSE‐ALPHA‐1, 3‐GALACTOSE: IMPLICATIONS BEYOND RED MEAT ALLERGIES. Internal Medicine Journal. 2017 Sep;47:24-.
41. Bradfisch F, Pietsch M, Forchhammer S, Strobl S, Stege HM, Pietsch R, Carstens S, Schäkel K, Yazdi A, Saloga J. Case series of anaphylactic reactions after rabies vaccinations with gelatin sensitization. Allergo Journal International. 2019 Jun 1;28(4):103-6.
42. Stone CA, Commins SP, Choudhary S, Vethody C, Heavrin JL, Wingerter J, Hemler JA, Babe K, Phillips EJ, Norton AE. Anaphylaxis after vaccination in a pediatric patient: further implicating alpha-gal allergy. The Journal of Allergy and Clinical Immunology: In Practice. 2019 Jan 1;7(1):322-4.
43. Stone CA, Hemler JA, Commins SP, Schuyler AJ, Phillips EJ, Peebles RS, Fahrenholz JM. Anaphylaxis after zoster vaccine: Implicating alpha-gal allergy as a possible mechanism. Journal of Allergy and Clinical Immunology. 2017 May 1;139(5):1710-3.
44. Pattanaik D, Lieberman P, Lieberman J, Pongdee T, Keene AT. The changing face of anaphylaxis in adults and adolescents. Annals of Allergy, Asthma & Immunology. 2018 Nov 1;121(5):594-7.
45. Ankersmit HJ, Copic D, Simader E. When meat allergy meets cardiac surgery: A driver for humanized bioprosthesis. The Journal of thoracic and cardiovascular surgery. 2017 Oct 1;154(4):1326-7.
46. Hawkins RB, Frischtak HL, Kron IL, Ghanta RK. Premature bioprosthetic aortic valve degeneration associated with allergy to galactose‐alpha‐1, 3‐galactose. Journal of cardiac surgery. 2016 Jul;31(7):446-8.
47. Kleiman AM, Littlewood KE, Groves DS. Delayed anaphylaxis to mammalian meat following tick exposure and its impact on anesthetic management for cardiac surgery: a case report. A&A Practice. 2017 Apr 1;8(7):175-7.
48. Mozzicato SM, Tripathi A, Posthumus JB, Platts-Mills TA, Commins SP. Porcine or bovine valve replacement in three patients with IgE antibodies to the mammalian oligosaccharide galactose-alpha-1, 3-galactose. The journal of allergy and clinical immunology. In practice. 2014 Sep;2(5):637.
49. Mangold A, Szerafin T, Hoetzenecker K, Hacker S, Lichtenauer M, Niederpold T, Nickl S, Dworschak M, Blumer R, Auer J, Ankersmit HJ. Alpha-Gal specific IgG immune response after implantation of bioprostheses. The Thoracic and cardiovascular surgeon. 2009 Jun;57(04):191-5.
50. Fischer J, Eberlein B, Hilger C, Eyer F, Eyerich S, Ollert M, Biedermann T. Alpha‐gal is a possible target of IgE‐mediated reactivity to antivenom. Allergy. 2017 May;72(5):764-71.
51. Rizer J, Brill K, Charlton N, King J. Acute hypersensitivity reaction to Crotalidae polyvalent immune Fab (CroFab) as initial presentation of galactose-α-1, 3-galactose (α-gal) allergy. Clinical Toxicology. 2017 Aug 9;55(7):668-9.
52. Farooque S, Kenny M, Marshall SD. Anaphylaxis to intravenous gelatin‐based solutions: a case series examining clinical features and severity. Anaesthesia. 2019 Feb;74(2):174-9.
53. Lied GA, Lund KB, Storaas T. Intraoperative anaphylaxis to gelatin-based hemostatic agents: a case report. Journal of asthma and allergy. 2019;12:163.
54. Tobacman JK. The common food additive carrageenan and the alpha-gal epitope. Journal of Allergy and Clinical Immunology. 2015 Dec 1;136(6):1708-9.
55. Tarlo SM, Dolovich J, Listgarten C. Anaphylaxis to carrageenan: A pseudo–latex allergy. Journal of allergy and clinical immunology. 1995 May 1;95(5):933-6.
56. Steinke JW, Platts-Mills TAE, Schuyler A, Commins SP. Reply to “The common food additive carrageenan and the alpha-gal epitope”. Journal of Allergy and Clinical Immunology. 2015 Oct 28;136(6):1709-10
57. Commins SP. Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients. Expert Review of Clinical Immunology. 2020 Jul 9:1-1.
58. Galili, U., & Avila, J. L. (Eds.). (2012). α–Gal and Anti–Gal: α1, 3–Galactosyltransferase, α–Gal Epitopes, and the Natural Anti–Gal Antibody Subcellular Biochemistry (Vol. 32). Springer Science & Business Media.
59. Fischer J, Lupberger E, Hebsaker J, Blumenstock G, Aichinger E, Yazdi AS, Reick D, Oehme R, Biedermann T. Prevalence of type I sensitization to alpha‐gal in forest service employees and hunters. Allergy. 2017 Oct;72(10):1540-7.
60. SAT0456 SERO-REACTIVITY TO GALACTOSE-ALPHA-1,3-GALACTOSE AND CLINICAL PRESENTATIONS OF PATIENTS SEEN IN A RHEUMATOLOGY OUTPATIENT PRACTICE. Annals of the Rheumatic Diseases 2019 Jun 15;78:1317-8.
61. Bianchi J, Walters A, Fitch ZW, Turek JW. Alpha-gal syndrome: Implications for cardiovascular disease. Global Cardiology Science and Practice. 2020 Feb 9;2019(3).
62. Carter MC, Ruiz‐Esteves KN, Workman L, Lieberman P, Platts‐Mills TA, Metcalfe DD. Identification of alpha‐gal sensitivity in patients with a diagnosis of idiopathic anaphylaxis. Allergy. 2018 May;73(5):1131-4.
63. Binder AM, Commins SP, Altrich ML, et al. Diagnostic testing for galactose-alpha-1,3-galactose, United States, 2010 to 2018. Ann Allergy Asthma Immunol. 2021;126(4):411-416.e1.
64. I-TICK Surveillance. Retrieved from: https://twitter.com/ITickUIUC/status/1282799807996854278
65. Wickner PG, Commins SP. The first 4 Central American cases of delayed meat allergy with galactose-alpha-1, 3-galactose positivity clustered among field biologists in Panama. Journal of Allergy and Clinical Immunology. 2014 Feb 1;133(2):AB212.
66. Ohshita N, Ichimaru Y, Gamoh S, Tsuji K, Kishimoto N, Tsutsumi YM, Momota Y. Management of infusion reactions associated with cetuximab treatment: A case report. Molecular and Clinical Oncology. 2017 Jun 1;6(6):853-5.
67. Stein D, Schuyler A, Commins S, Behm B, Chitnavis M. P-002 YI First Dose IgE-Mediated Allergy to Infliximab Due to Galactose-α-1, 3-Galactose Allergy. Inflammatory Bowel Diseases. 2016 Mar 1;22:S9-10.
68. Van Tine BA, Govindarajan R, Attia S, Somaiah N, Barker SS, Shahir A, Barrett E, Lee P, Wacheck V, Ramage SC, Tap WD. Incidence and management of olaratumab infusion-related reactions. Journal of oncology practice. 2019 Nov;15(11):e925-33.
69. Venturini M, Lobera T, Sebastián A, Portillo A, Oteo JA. IgE to α-Gal in Foresters and Forest Workers From La Rioja, North of Spain. Journal of investigational allergology & clinical immunology. 2018;28(2):106.
70. Apostolovic D, Tran TA, Hamsten C, Starkhammar M, Cirkovic Velickovic T, van Hage M. Immunoproteomics of processed beef proteins reveal novel galactose‐α‐1, 3‐galactose‐containing allergens. Allergy. 2014 Oct;69(10):1308-15.
71. Khora SS, Navya P. Bioactive Polysaccharides from Marine Macroalgae. Encyclopedia of Marine Biotechnology. 2020 Aug 4.
72. Gowda DC, Glushka J, Halbeek HV, Thotakura RN, Bredehorst R, Vogel CW. N-linked oligosaccharides of cobra venom factor contain novel α (1-3) galactosylated Lex structures. Glycobiology. 2001 Mar 1;11(3):195-208.
73. Hodžić A, Mateos-Hernández L, Fréalle E, Román-Carrasco P, Alberdi P, Pichavant M, Risco-Castillo V, Le Roux D, Vicogne J, Hemmer W, Auer H. Infection with Toxocara canis Inhibits the Production of IgE Antibodies to α-Gal in Humans: Towards a Conceptual Framework of the Hygiene Hypothesis?. Vaccines. 2020 Jun;8(2):167.
74. Taguchi T, Kitajima K, Muto Y, Inoue S, Khoo KH, Morris HR, Dell A, Wallace RA, Selman K, Inoue Y. A precise structural analysis of a fertilization-associated carbohydrate-rich glycopeptide isolated from the fertilized eggs of euryhaline killi fish (Fundulus heteroclitus). Novel penta-antennary N-glycan chains with a bisecting N-acetylglucosaminyl residue. Glycobiology. 1995 Sep 1;5(6):611-24.
75. Shao Y, Yu Y, Pei CG, Qu Y, Gao GP, Yang JL, Zhou Q, Yang L, Liu QP. The expression and distribution of α-Gal gene in various species ocular surface tissue. International journal of ophthalmology. 2012;5(5):543.
76. Chauhan PS, Saxena A. Bacterial carrageenases: an overview of production and biotechnological applications. 3 Biotech. 2016 Dec 1;6(2):146.
77. USDA Carrageenan Handling/Processing
78. van Nunen S. Galactose-alpha-1, 3-galactose, mammalian meat and anaphylaxis: a world-wide phenomenon?. Current Treatment Options in Allergy. 2014 Sep 1;1(3):262-77.
79. Wilson JM, Nguyen AT, Schuyler AJ, Commins SP, Taylor AM, Platts-Mills TA, McNamara CA. IgE to the mammalian oligosaccharide galactose-α-1, 3-galactose is associated with increased atheroma volume and plaques with unstable characteristics—brief report. Arteriosclerosis, thrombosis, and vascular biology. 2018 Jul;38(7):1665-9.
80. Wilson JM, McNamara CA, Platts-Mills TA. IgE, α-Gal and atherosclerosis. Aging (Albany NY). 2019 Apr 15;11(7):1900.
81. Tina Merritt, MD, personal communication.
82. Hodgeman N, Horn CL, Paredes A. An Unusual Mimicker of Irritable Bowel Disease: 1855. American Journal of Gastroenterology. 2019 Oct 1;114(2019 ACG Annual Meeting Abstracts):S1039.
83. Bensinger A, Green P. Mammalian Meat Allergy Masquerading as IBS-D: 1846. American Journal of Gastroenterology. 2019 Oct 1;114(2019 ACG Annual Meeting Abstracts):S1036-7.
84. Mabelane T, Basera W, Botha M, Thomas HF, Ramjith J, Levin ME. Predictive values of alpha‐gal IgE levels and alpha‐gal IgE: Total IgE ratio and oral food challenge‐proven meat allergy in a population with a high prevalence of reported red meat allergy. Pediatric Allergy and Immunology. 2018 Dec;29(8):841-9.
85. Armstrong P, Binder A, Amelio C, Kersh G, Biggerstaff B, Beard C, Petersen L, Commins S. Descriptive Epidemiology of Patients Diagnosed with Alpha-gal Allergy—2010–2019. Journal of Allergy and Clinical Immunology. 2020 Feb 1;145(2):AB145.
86. Pointreau Y, Commins SP, Calais G, Watier H, Platts-Mills TA. Fatal infusion reactions to cetuximab: role of immunoglobulin E–mediated anaphylaxis. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2012 Jan 20;30(3):334.
87. van Nunen S. Tick-induced allergies: mammalian meat allergy, tick anaphylaxis and their significance. Asia Pacific Allergy. 2015 Jan 1;5(1):3-16.
88. van Nunen S, O’Connor K, Fernando S, Clarke L, Boyle R. THE ASSOCIATION BETWEEN IXODES HOLOCYCLUS TICK BITE REACTIONS AND RED MEAT ALLERGY: P17. Internal Medicine Journal. 2007 Nov 1;37.
89. Van Nunen SA, O’Connor KS, Clarke LR, Boyle RX, Fernando SL. An association between tick bite reactions and red meat allergy in humans. The Medical journal of Australia. 2009 May 4;190(9):510-1.
90. Meat Allergy Tirggered by a Tick Bite with Eri McGintee retrieved from: https://youtu.be/hj96Vvr1WhQ
91. Fischer J, Huynh HN, Hebsaker J, Forchhammer S, Yazdi AS. Prevalence and Impact of Type I Sensitization to Alpha-Gal in Patients Consulting an Allergy Unit. International Archives of Allergy and Immunology. 2020;181(2):119-27.
92. Platts-Mills TA, Commins SP, Biedermann T, van Hage M, Levin M, Beck LA, Diuk-Wasser M, Jappe U, Apostolovic D, Minnicozzi M, Plaut M. On the cause and consequences of IgE to galactose-α-1, 3-galactose: a Report from the National Institute of Allergy and Infectious Disease Workshop on Understanding IgE-Mediated Mammalian Meat Allergy. Journal of Allergy and Clinical Immunology. 2020 Feb 10.
93. Takahashi H, Chinuki Y, Tanaka A, Morita E. Laminin γ‐1 and collagen α‐1 (VI) chain are galactose‐α‐1, 3‐galactose–bound allergens in beef. Allergy. 2014 Feb;69(2):199-207.
94. Hilger C, Fischer J, Swiontek K, Hentges F, Lehners C, Eberlein B, Morisset M, Biedermann T, Ollert M. Two galactose‐α‐1, 3‐galactose carrying peptidases from pork kidney mediate anaphylactogenic responses in delayed meat allergy. Allergy. 2016 May;71(5):711-9.
95. Iweala OI, Choudhary SK, Addison CT, Batty CJ, Kapita CM, Amelio C, Schuyler AJ, Deng S, Bachelder EM, Ainslie KM, Savage PB. Glycolipid-mediated basophil activation in alpha-gal allergy. Journal of Allergy and Clinical Immunology. 2020 Feb 20.
96. Iweala O, Brennan PJ, Commins SP. Serum IgE specific for alpha-Gal sugar moiety can bind glycolipid. Journal of Allergy and Clinical Immunology. 2017 Feb 1;139(2):AB88.
97. Iweala OI, Choudhary SK, Addison CT, Batty CJ, Kapita CM, Amelio C, Schuyler AJ, Deng S, Bachelder EM, Ainslie KM, Savage PB. Glycolipid-mediated basophil activation in alpha-gal allergy. Journal of Allergy and Clinical Immunology. 2020 Feb 20.
98. Villalta D, Pantarotto L, Da Re M, Conte M, Sjolander S, Borres MP, Martelli P. High prevalence of sIgE to Galactose‐α‐1, 3‐galactose in rural pre‐Alps area: a cross‐sectional study. Clinical & Experimental Allergy. 2016 Feb;46(2):377-80.
99. Galili U, Clark MR, Shohet SB, Buehler J, Macher BA. Evolutionary relationship between the natural anti-Gal antibody and the Gal alpha 1—-3Gal epitope in primates. Proceedings of the National Academy of Sciences. 1987 Mar 1;84(5):1369-73.
100. Wilson JM, Platts-Mills TA. The oligosaccharide galactose-α-1, 3-galactose and the α-Gal syndrome: insights from an epitope that is causal in immunoglobulin E-mediated immediate and delayed anaphylaxis. Eur Med J. 2018;3:89-98.
101. Zurbano-Azqueta L, Antón-Casas E, Duque-Gómez S, Jiménez-Gómez I, Fernández-Pellón L, López-Gutiérrez J. Alpha-gal syndrome. Allergy to red meat and gelatin. Revista Clínica Española (English Edition). 2021 Oct 14.
102. Christian RA, Stabile KJ, Gupta AK, Leckey Jr BD, Cardona DM, Nowinski RJ, Kelly JD, Toth AP. Histologic Analysis of Porcine Dermal Graft Augmentation in Treatment of Rotator Cuff Tears. The American journal of sports medicine. 2021 Oct 15:03635465211049434.
103. Kuravi KV, Sorrells LT, Nellis JR, et al. Allergic response to medical products in patients with alpha-gal syndrome. J Thorac Cardiovasc Surg. Published online April 9, 2021. doi:10.1016/j.jtcvs.2021.03.100
104. Chinuki Y, Morita E, Takahashi H. IgE antibodies to galactose-a-1,3-galactose, an epitope of red meat allergen, cross-react with a novel flounder roe allergen. J Investig Allergol Clin Immunol. Published online October 15, 2021:0.
105. Shao Y, Yu Y, Pei C-G, et al. The expression and distribution of α-Gal gene in various species ocular surface tissue. Int J Ophthalmol. 2012;5(5):543.
106. Murangi T, Prakash P, Moreira BP, et al. Ascaris lumbricoides and ticks associated with sensitisation to Galactose α1,3-galactose and elicitation of the alpha-gal syndrome. J Allergy Clin Immunol. Published online July 29, 2021. doi:10.1016/j.jaci.2021.07.018
107. Mateos-Hernández L, Risco-Castillo V, Torres-Maravilla E, et al. Gut Microbiota Abrogates Anti-α-Gal IgA Response in Lungs and Protects against Experimental Aspergillus Infection in Poultry. Vaccines (Basel). 2020;8(2). doi:10.3390/vaccines8020285
108. Aspergillus oryzae, Wikipedia
109. Murugan AVM, Oliveira T, Alagesan K, et al. Evolutionary Glycomics: A Comprehensive Study of Vertebrate Host Serum/Plasma Glycome Using Orthogonal Glycomics Techniques. The FASEB Journal. 2021;35(S1). doi:10.1096/fasebj.2021.35.S1.04538
110. Gowda DC, Glushka J, van Halbeek H, Thotakura RN, Bredehorst R, Vogel C-W. N-linked oligosaccharides of cobra venom factor contain novel α (1-3) galactosylated Lex structures. Glycobiology. 2001;11(3):195-208.
111. Ramasamy R. Mosquito vector proteins homologous to α1-3 galactosyl transferases of tick vectors in the context of protective immunity against malaria and hypersensitivity to vector bites. Parasit Vectors. 2021;14(1):303.
112. Fukunaga T, Tanaka N, Furumoto T, et al. Substrate specificities of α1,2- and α1,3-galactosyltransferases and characterization of Gmh1p and Otg1p in Schizosaccharomyces pombe. Glycobiology. Published online April 28, 2021. doi:10.1093/glycob/cwab028
113. van Nunen, S. Mammalian Meat Allergy after Tick Bite and Tick Anaphylaxis in Australia. International Tick Symposium (2018). 2018. Retrieved from https://www.youtube.com/watch?v=C4fzZO9UlzE&list=LLcoL9fUr713IGKBwo-CELVw&index=21 @1:09:00
114. Scott Commins, MD, PhD, personal communication
115. Perusko M, Apostolovic D, Kiewiet MB, Grundström J, Hamsten C, Starkhammar M, Cirkovic Velickovic T, van Hage M. Bovine γ‐globulin, lactoferrin, and lactoperoxidase are relevant bovine milk allergens in patients with α‐Gal syndrome. Allergy. 2021 May 3.
116. Croglio MP, Commins SP, McGill SK. Isolated Gastrointestinal Alpha-gal Meat Allergy Is a Cause for Gastrointestinal Distress Without Anaphylaxis. Gastroenterology. 2021 May 1;160(6):2178-80.
117. Richards NE, Richards Jr RD. Alpha-Gal Allergy as a Cause of Intestinal Symptoms in a Gastroenterology Community Practice. Southern Medical Journal. 2021 Mar 1;114(3):169-73.
