What to Do If You Are Bitten by a Tick
A Guide for People with Alpha-gal Syndrome
Tick Removal
How NOT to Remove Ticks
Improper tick removal may increase your risk of developing AGS and tick-borne diseases.
- Do NOT agitate ticks or squeeze their abdomens; this may cause them to eject saliva into the bite site.
- Do NOT apply heat to the ticks or burn them with a hot match.
- Do NOT cover ticks with petroleum jelly, nail polish, alcohol, gasoline or essential oils.
- Do NOT use your bare fingers to remove ticks.
- Do NOT twist the body of the tick.
- Do NOT use blunt, household tweezers. Use sharp, pointy ones.

Do NOT twist ticks

Do NOT burn ticks

Do NOT squeeze ticks
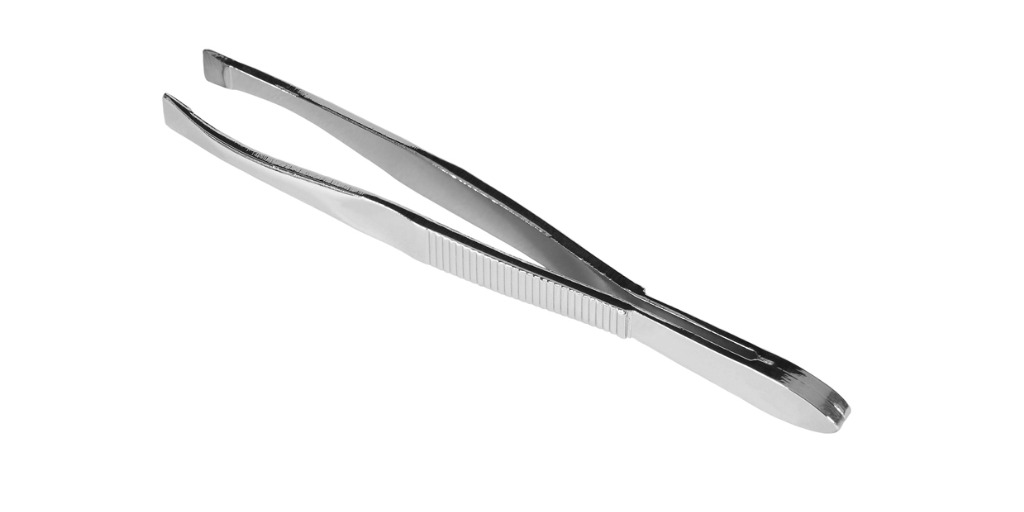
Do NOT use blunt tweezers to remove ticks

Do NOT smother ticks
Do NOT use bare fingers to remove ticks
How to Correctly Remove Ticks, from the CDC:
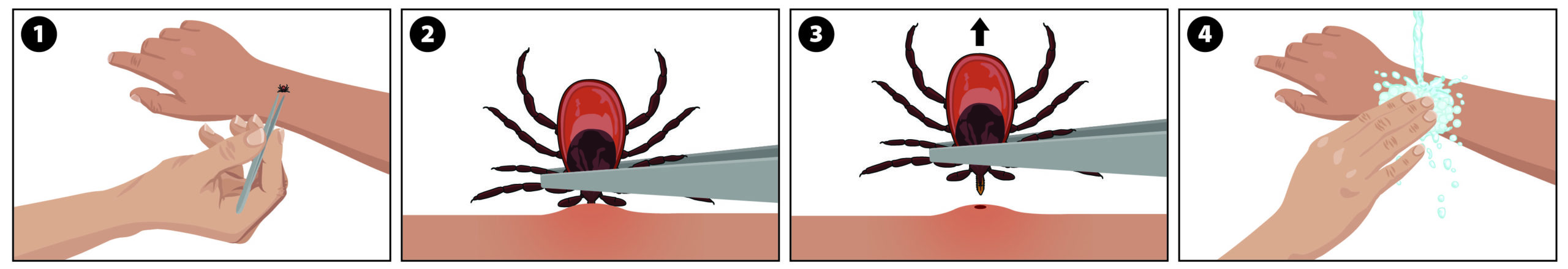
If you find a tick attached to your skin, there’s no need to panic—the key is to remove the tick as soon as possible. There are several tick removal devices on the market, but a plain set of fine-tipped tweezers work very well.
How to remove a tick
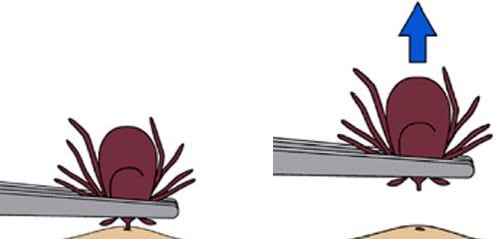
- Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
- Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouth-parts to break off and remain in the skin. If this happens, remove the mouth-parts with tweezers. If you are unable to remove the mouth easily with clean tweezers, leave it alone and let the skin heal.
- After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
- Never crush a tick with your fingers. Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet.
Follow up
If you develop a rash or fever within several weeks of removing a tick, see your doctor. Be sure to tell the doctor about your recent tick bite, when the bite occurred, and where you most likely acquired the tick.
Source: CDC Tick Removal


Source: CDC Tick Removal
Where to Find Tick Tweezers
Any sharp, pointed tweezers will do, but TickEase tweezers are a popoular choice.
TERC How to Remove a Tick Video
Dos and Don’ts of Tick Removal
How to remove a tick, from TickEase tick removal expert Tick Man Dan.
Freezing Ticks
Australian AGS expert Dr. Sheryl van Nunen proposes a tick removal method that involves freezing ticks prior to removing them. This method has not been tested on North American ticks and is not endorsed by the CDC for use in the United States.
After Removing Ticks
Immediately After Tick Removal
- Clean the bite area and wash your hands with rubbing alcohol or soap and water.
- Consider photographing the tick to help with identifying the species.
- If you do not save the tick, flush it down the toilet.
CDC Factsheet
What to do after a tick bite PDF
Saving Ticks
- Consider saving any ticks you remove in order to either send them to a lab to be identified and tested or in case you develop any tick-borne diseases and want additional information about them at that point.
- Use one of these methods:
- Tape the tick securely to a card. Record the date and location of the bite on the card. Put the card in an airtight bag or container
- Put the tick in a sealed container of rubbing alcohol.
- Put the tick in a closed and labeled baggie in the freezer.
- Record the date and location of tick bites in your calendar. Record the species of tick, if you know it. This information may be helpful to your doctor.
Calling Your Health Provider
- Consider calling your healthcare provider for advice about prophylactic antibiotics.
- In some cases, a single dose of doxycycline after a tick bite may lower your risk of aquiring Lyme Disease.
- Do not delay, call the day you are bitten or as soon as possible, as prophylactic antibiotics need to be taken promptly.
Tick Identification
Tick Identification
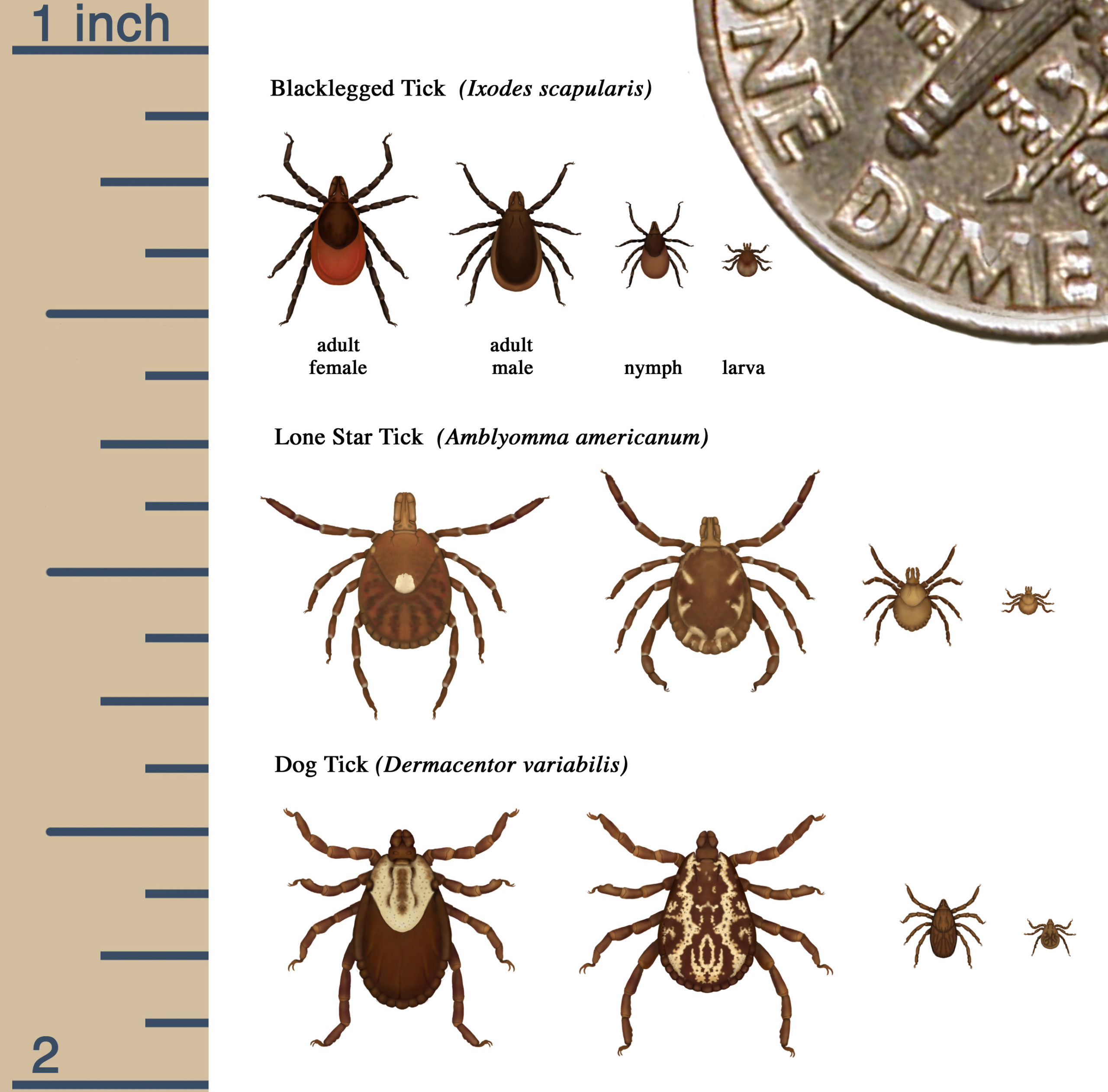
Different species of ticks transmit different diseases. Some are associated with alpha-gal syndrome and some aren’t. For this reason, you may want to identify any ticks that bite you.
- The CDC provides information on tick species and their distribution on here.
- Information about identifying ticks can be found here..
- The CDC also has a Tick Image Gallery.
- There are many websites with good information about tick identification. One of our favorites is the TERC website.
- You can buy tick identification cards to keep with you when you go outside here.
- If you take a good photo of the tick that bites you, you can send it to TickSpotters to be identified.
Information about ticks associated with alpha-gal syndrome is available here.
Tick Lifecycles
Source: CDC
Lone Star Tick Image Gallery
Click images to enlarge
Lone Star Tick (Amblyomma americanum)* female
Source: CDC
*Strongly associated with AGS in U.S.
Lone Star Tick (Amblyomma americanum)* male
Source: CDC
*Strongly associated with AGS in U.S.
Lone Star Tick (Amblyomma americanum)* nymph
Source: CDC
*Strongly associated with AGS in U.S.
Lone Star Tick (Amblyomma americanum)* engorged female with eggs
Source: CDC
*Strongly associated with AGS in U.S.
Other Possible North American Vectors
Ticks
Asian Longhorned Tick (Haemaphysalis longicornis)* female
Source: CDC
*Associated with AGS in Asia and likely to be associated with AGS in U.S.
American Dog Tick (Dermacentor variabilis)* female
Source: CDC
*Anecdotally associated with AGS in Wisconsin and Minnesota
Cayenne Tick (Amblyomma cajennense)* female
Source: CDC
*Associated with AGS in Central America, but also found in Texas and Florida
Blacklegged Tick (Ixodes scapularis)* female
Source: CDC
*As of yet, not associated with AGS, but has alpha-gal in its saliva
Mites
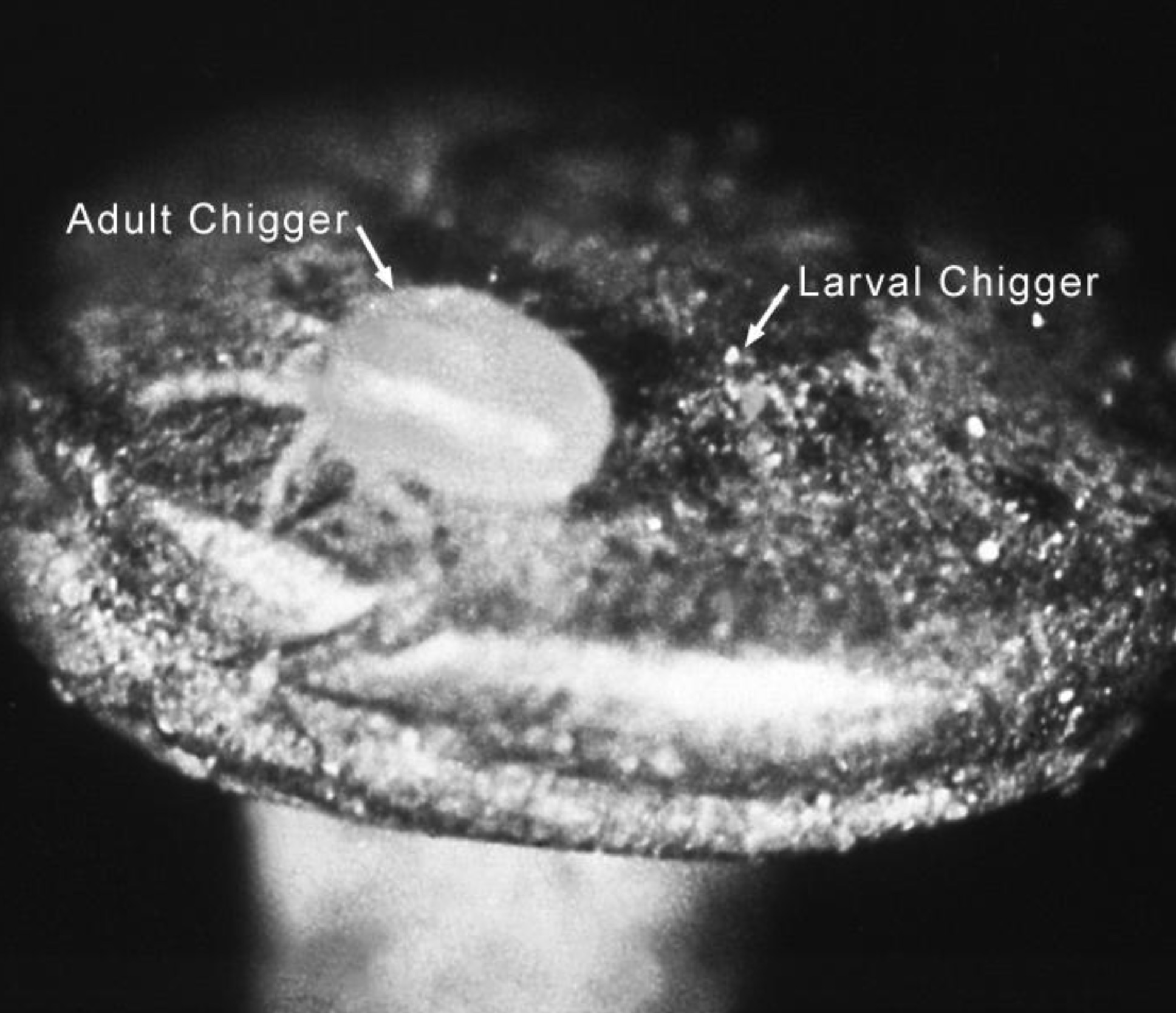
Chigger (Trombicula sp.) adult and larva on the head of a pin
Source: CDC
*There is speculation that chiggers may trigger AGS. Note that it is the larvae of chiggers that feed on humans, not the adults. The larvae are 0.17-0-.22mm in diameter, a size barely detectable by the naked eye. If you can see what bit you, it is probably not a chigger; it is most likely a larval tick. Larval ticks are also tiny, but visible.
Tick Testing
How to Get a Tick Tested
- The CDC strongly recommends against using tick test results to decide whether to use antibiotics after a tick bite (see below). Nonetheless, having the ticks you remove tested can still provide you with useful information, such as:
- The species of tick.
- Disease-causing organisms and viruses that the tick may be carrying.
- For more information about tick testing see:
- Some of the companies that test ticks include:
Tick Testing, from the CDC:
People who have removed a tick sometimes wonder if they should have it tested for evidence of infection. Although some commercial groups offer testing, in general this is not recommended because:
- Laboratories that conduct tick testing are not required to have the high standards of quality control used by clinical diagnostic laboratories. Results of tick testing should not be used for treatment decisions.
- Positive results showing that the tick contains a disease-causing organism do not necessarily mean that you have been infected.
- Negative results can lead to false assurance. You may have been unknowingly bitten by a different tick that was infected.
- If you have been infected, you will probably develop symptoms before results of the tick test are available. If you do become ill, you should not wait for tick testing results before beginning appropriate treatment.
Source: CDC Testing of Ticks
Watch for Symptoms of Tick-borne Disease
The CDC recommends watching for the following symptoms of tick-borne disease for 30 days after tick bites:
- Rash
- Headache
- Fever
- Fatigue
- Muscle pain
- Joint swelling and pain
If you develop any of these symptoms, contact your healthcare provider for advice.
For more information see the CDC Symptoms of Tickborne Illness.
Monitor Alpha-gal Allergy Reactions
People Who Do Not Have Alpha-gal Syndrome:
- Most people who are bitten by ticks do not develop alpha-gal syndrome.
- Most experts do not recommend routine testing for sensitization to alpha-gal after tick bites. This is because many people will test positive for alpha-gal IgE after a bite, but most will not develop alpha-gal syndrome.
- Don’t expect to know whether your tick bite triggered AGS immediately. Alpha-gal syndrome can take weeks or even months to develop. Six weeks to two months is typical for many of us, although sometimes onset is faster.
- If you were bitten by a known or suspected vector of alpha-gal syndrome, you may want to be careful about what you eat for awhile.
- Note any symptoms, the date and time of day when they occur, and what foods and medications you consumed during the twelve hours before their onset. Written records and photographs will help your physician diagnose you.
- Keep in mind that the symptoms of AGS and other tick-borne diseases can overlap. Even if you develop AGS, don’t assume that all the symptoms you experience afterwards are caused by it. Talk to your healthcare provider about ruling out tick-borne diseases and other illnesses that may be contributing to your symptoms.
- Seek the advice of a physician, not strangers on Facebook.
- Many people with AGS find that their healthcare providers know little about it. They figure out that they have it themselves and find a specialist on their own. Many are given the wrong tests, when their healthcare providers are willing to test them at all. Don’t go to your doctor’s appointment unprepared: bring information about AGS and the test codes for the Alpha-gal Panel.
- There is more information on how to prepare for an appointment with a healthcare provider to discuss AGS here.
- If your healthcare provider is unfamiliar with AGS and uninterested in learning about it, try to make an appointment with an expert or patient-recommended physician.
I remember finding what I thought was a dog tick on my belly and thinking, “Oh good! It is not a deer tick! I don’t have to worry about Lyme with this one!” HA! Five weeks later, I woke in a full body rash. Four additional weeks later, I was diagnosed with Alpha Gal. Life has been on an unchartered course ever since. However, I remain hopeful and positive!
People Who Already Have Alpha-gal Syndrome:
- Tick bites can maintain or lead to increases in the alpha-gal IgE of people with AGS.
- If you already have AGS and are bitten by another tick:
- You may become more sensitive to alpha-gal.
- Your threshold for reactivity may be lowered, meaning that you may react to smaller amounts of alpha-gal.
- You may have to give up foods that you previously tolerated, like dairy, gelatin, or products that contain other ingredients made from mammals.
- Multiple tick bites are even more likely to lead to increased sensitivity.
- Watch for changes in your reactions and take extra precautions in the months following a tick bite.
- Keep in mind that the symptoms of AGS and other tick-borne diseases can overlap. Don’t assume that new symptoms that develop after tick bites are caused by AGS. Talk to your healthcare provider about ruling out tick-borne diseases and other illnesses that may be contributing to your symptoms.
More Information

Ticks and Alpha-gal Syndrome→

Avoiding Tick Bites→

Ticks and Pets→

Symptoms of AGS→

Diagnosis of AGS→

Physician Experts→
Additional Resources
General Information
CDC Ticks
Tick Encounter Resource Center
TIC NC
Testing
Ticknology
Tick Encounter Resource Center
Save the Tick
Tick Report
References
1. CDC Ticks
2. Tick Encounter Resource Center
3. Commins SP. Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients. Expert Review of Clinical Immunology. 2020 Jul 9:1-1.
All the information on alphagalinformation.org is provided in good faith, but we, the creators and authors of the Alpha-gal Information website offer no representation or warranty, explicit or implied, of the accuracy, adequacy, validity, reliability, availability, or completeness of any information on this site. Under no circumstances should we have any liability for any loss or damage incurred by you as a result of relying on information provided here. We are not physicians or medical professionals, researchers, or experts of any kind. Information provided in this website may contain errors and should be confirmed by a physician. Information provided here is not medical advice. It should not be relied upon for decisions about diagnosis, treatment, diet, food choice, nutrition, or any other health or medical decisions. For advice about health or medical decisions including, but not limited to, diagnosis, treatment, diet, and health care consult a physician.
READ FULL DISCLAIMER>