Diagnosis and Testing
A Patient Guide to the Diagnosis of Alpha-gal Syndrome
Update
When this website was created, there wasn’t an up-to-date, comprehensive guide to the diagnosis and management of alpha-gal syndrome (AGS). Now two have been published, both written by leading experts. In addition, there is an excellent paper comparing AGS and other forms of mammalian meat allergy. If you are a healthcare provider, or even a patient with a more than casual interest in alpha-gal syndrome, you will want to read these papers. Although this page draws heavily from these publications, it is not a substitute for them.
Key papers on the diagnosis and management of alpha-gal syndrome
- Commins SP. Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients. Expert Review of Clinical Immunology. 2020 Jul 9:1-1.
- Platts-Mills TA, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-Gal syndrome. The Journal of Allergy and Clinical Immunology: In Practice. 2020 Jan 1;8(1):15-23.
Key paper comparing AGS and other mammalian meat allergies
- Wilson JM, Platts-Mills TA. Red meat allergy in children and adults. Current opinion in allergy and clinical immunology. 2019 Jun 1;19(3):229-35.
Allergies to Mammalian Meat
Red meat, at least in some populations, is a major food allergen (17).
There is more than one mammalian meat allergy. These allergies differ from each other in significant ways. The three dominant forms of mammalian meat allergy are (17):
- Alpha-gal syndrome: an allergy to the sugar galactose-alpha-1,3-galactose (alpha-gal) in mammalian meat, other parts of mammals, and products derived from them (3)
- Primary beef allergy (20)
- Pork-cat syndrome: an allergy to pork caused by exposure to cats (22, 23)
In addition, about 20% of children with milk allergy experience reactions after eating beef (19, 21).
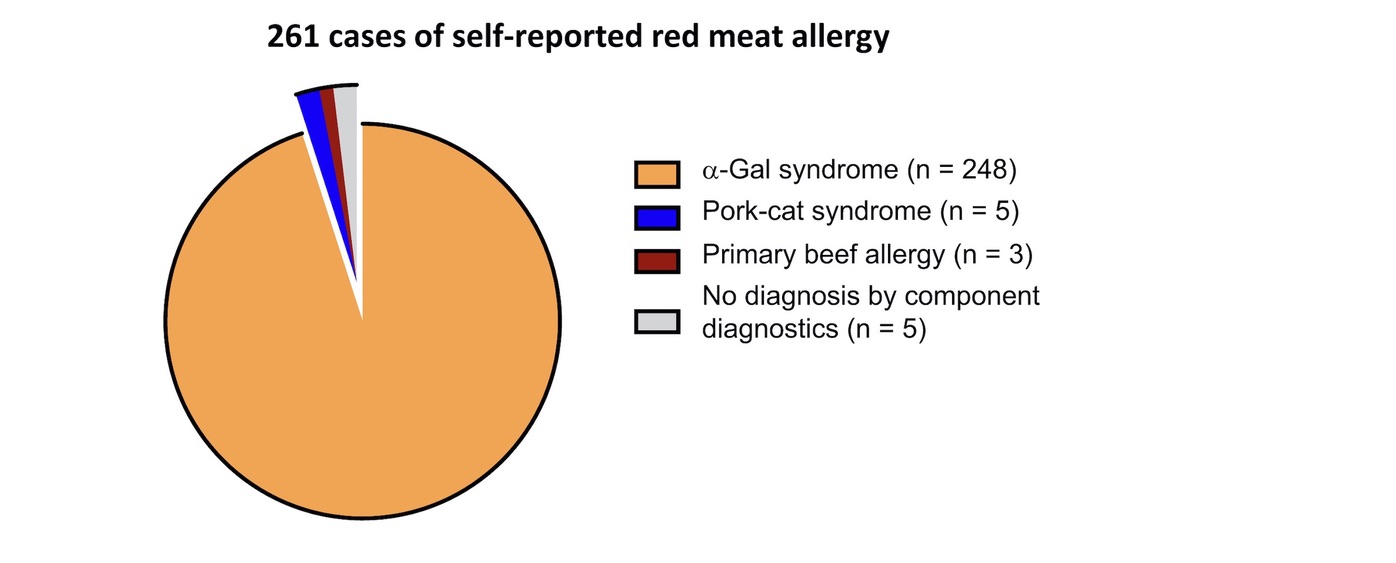
Figure 1. Distribution of component-based diagnoses of 261 cases of self-reported mammalian meat allergy. Reproduced with permission from Elsevier.
Source: Wilson JM, Schuyler AJ, Workman L, Gupta M, James HR, Posthumus J, McGowan EC, Commins SP, Platts-Mills TA. Investigation into the α-gal syndrome: characteristics of 261 children and adults reporting red meat allergy. The Journal of Allergy and Clinical Immunology: In Practice. 2019 Sep 1;7(7):2348-58.
How is Alpha-gal Syndrome Diagnosed?
In >90% of cases, the diagnosis of AGS can be made based on a history of delayed allergic reactions after eating non-primate mammalian meat (e.g. ‘red meat’ such as beef, pork, or lamb) and a positive blood test (>0.1 IU/mL) for IgE to alpha-gal. The combination of both an appropriate clinical history and supporting blood test is necessary to establish an accurate AGS diagnosis (2).
The different allergies to mammalian meat have different features (17). If you experience symptoms after eating mammalian meat, in most cases, your primary care physician or allergist should be able to determine whether you have alpha-gal syndrome; pork-cat syndrome; primary beef allergy; “traditional” cow’s milk allergy or a different health issue based on a combination of your clinical history and test results. If not, allergists at referral centers like UNC and UVA have experience diagnosing less straightforward cases (see Physician Experts).
Doctors diagnose alpha-gal syndrome through a combination of clinical history and tests, including:
- History of allergic reactions to mammalian meat, including symptoms, timing of symptoms, and age of onset (1,2)
- History of exposure to ticks, including the presence or absence of persistent, localized reactions to tick bites (1,2)
- A blood test for Galactose-alpha-1,3-galactose (alpha-gal) specific IgE (sIgE) (1,2)
- Responsiveness to dietary changes (1,2)
Skin prick tests with commercial extracts of beef or pork and are frequently negative or borderline positive. They are unreliable and not recommended for the diagnosis of alpha-gal syndrome (1,2,3,5).
Prick-to-prick (prick-prick) skin testing using raw or cooked meats/organs are also used in some cases (2,6,8,9). Please see Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients for more information about this method.
Intradermal (ID) testing with meat extracts or gelatin-derived medical products are sometimes used in the diagnostic process, especially when blood tests are negative but there is a history of delayed reactions after ingestion of mammalian meat (1,2,6,7). Some studies suggest ID testing with gelatin is more reliable than ID testing with meat extracts (2). However, intradermal testing involves risks and few clinics perform these tests (2).
Commins describes a multi-step protocol used by a referral center for diagnosing the 2% of patients with a history of reactions to mammalian products who test negative for alpha-gal IgE (2). This is detailed in Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients and can include:
- The assessment of surrogate markers (beef, pork, lamb) by skin and serum IgE testing (2)
- Testing for cat serum albumin (Fel d2) to identify patients with pork-cat syndrome (2)
- Testing for IgE to both porcine and bovine gelatin (2)
- Skin testing using alpha-gal-containing biologics such as cetuximab (2)
- Basophil activation testing (2,4)
This approach has led to diagnostic clarification in 78% of patients with seronegative testing who report compelling symptoms (2).
Occasionally, food challenges are used in diagnosis of AGS. Food challenges need to be conducted with the utmost care, because of the delayed and unpredictiable nature and severity of allergic reactions to alpha-gal. Commins reports that 15-20% of food challenge reactions in patients with AGS require one or more doses of epinephrine and/or emergency medical transport (2). In Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients Commins describes the limited set of circumstances in which alpha-gal food challenges are clinically appropriate (2) and makes recommendations as to how to conduct them.
Expert Scott Commins writes:
The following characteristics occur in 85% of patients with AGS:
(I) Onset in adult life after eating mammalian meat without problems for many years
(II) Reactions range from pruritus, localized hives or angioedema to anaphylaxis
(III) Patients can report strictly gastrointestinal symptoms (diarrhea, abdominal cramping, emesis) almost to the exclusion of cutaneous, cardiovascular, or respiratory manifestations
(IV) Reactions start 3–8 hours after eating non-primate mammalian meat (or consumption of dairy, gelatin, or other mammalian-derived products)
(V) Positive testing for alpha-gal IgE (>0.1 IU/mL)
(VI) Improvement of symptoms when adhering to an appropriate avoidance diet
(VII) Description of large local reactions to tick or other arthropod bites, often including report of an ‘index’ bite that behaved differently than prior bites (2)
Expert Scott Commins writes:
In terms of diagnosis, skin prick tests with extracts of mammalian meats (beef, pork, or lamb) were shown to be unreliable (2).
Expert Thomas Platts-Mills, et al write:
In terms of diagnosis it became clear in early studies that prick tests with extracts of beef or pork were unreliable (1).
Expert Thomas Platts-Mills, et al write:
The final element of diagnosis depends on how they respond clinically to a diet avoiding red meat (1).
What Blood Tests Do Doctors Use to Help Them Diagnose Alpha-gal Syndrome?
With a convincing clinical history, alpha-gal IgE levels at least 0.1 kU/l confirm the diagnosis of alpha-gal syndrome. With a murky clinical history, some have argued that an alpha-gal IgE at least 2 kU/l or at least 2% of the total IgE should be used to confirm the diagnosis of alpha-gal syndrome (5).
Alpha-gal IgE
A blood test for galactose-alpha-1,3-galactose (alpha-gal) specific IgE (sIgE) is the main test that healthcare providers use to help them diagnose alpha-gal syndrome (1,2). In the U.S., this test is available via Viracor Eurofins Clinical Diagnostics. In Europe, it is available via Phadia Thermofisher.
Viracor (U.S.)
Below is a link to a Viracor website page with information about the test for galactose-alpha-1,3-galactose (alpha-gal) sIgE and the test code they use.
- Galactose-alpha-1,3 galactose (Alpha-Gal) IgE
Test Code: 30039 - Unless a provider has a contract with Viracor (and few do) they will typically send patients to a commercial lab, like Quest or Labcorp, which send samples to Viracor to be tested.
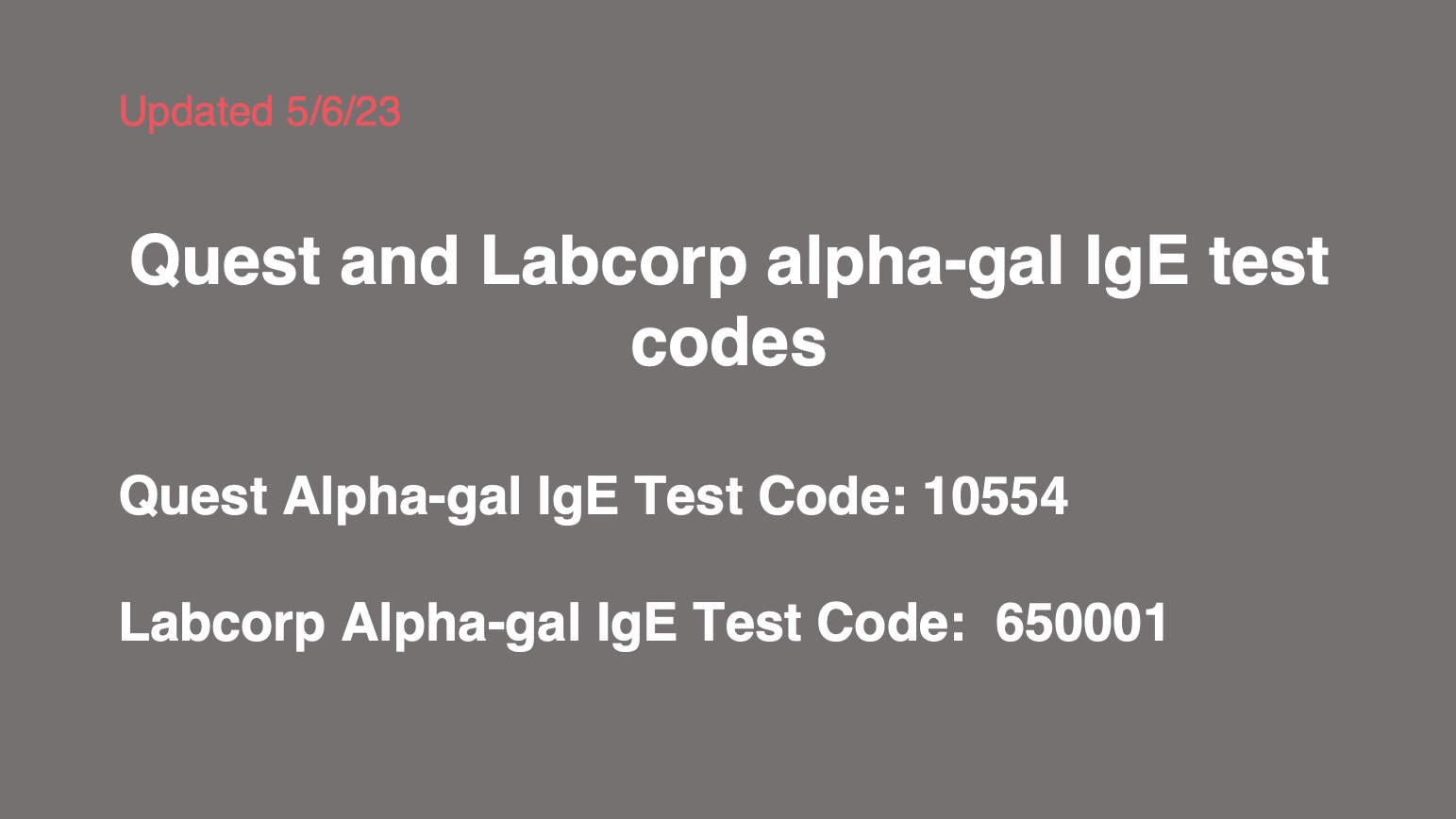
Quest and Labcorp (U.S.)
- Both Quest and Labcorp can send your blood samples to Viracor, if your doctor gives them the right codes. Many doctors struggle to find these test codes on their own, especially the Labcorp codes. Often, they use the wrong codes.
- Double-check the below codes using the links provided, in case they change.
- Take a copy of the test codes with you to your appointment. See the printable PDF below.
- Quest Galactose-alpha-1,3-galactose (Alpha-gal) IgE Test Code: 10554
- Labcorp Galactose-alpha-1,3-galactose (Alpha-gal) IgE Test Code: 650001 (As of 12/13/21 Labcorp reported a cost of $77 for this test)
Phadia Thermofisher (Europe)
Australia
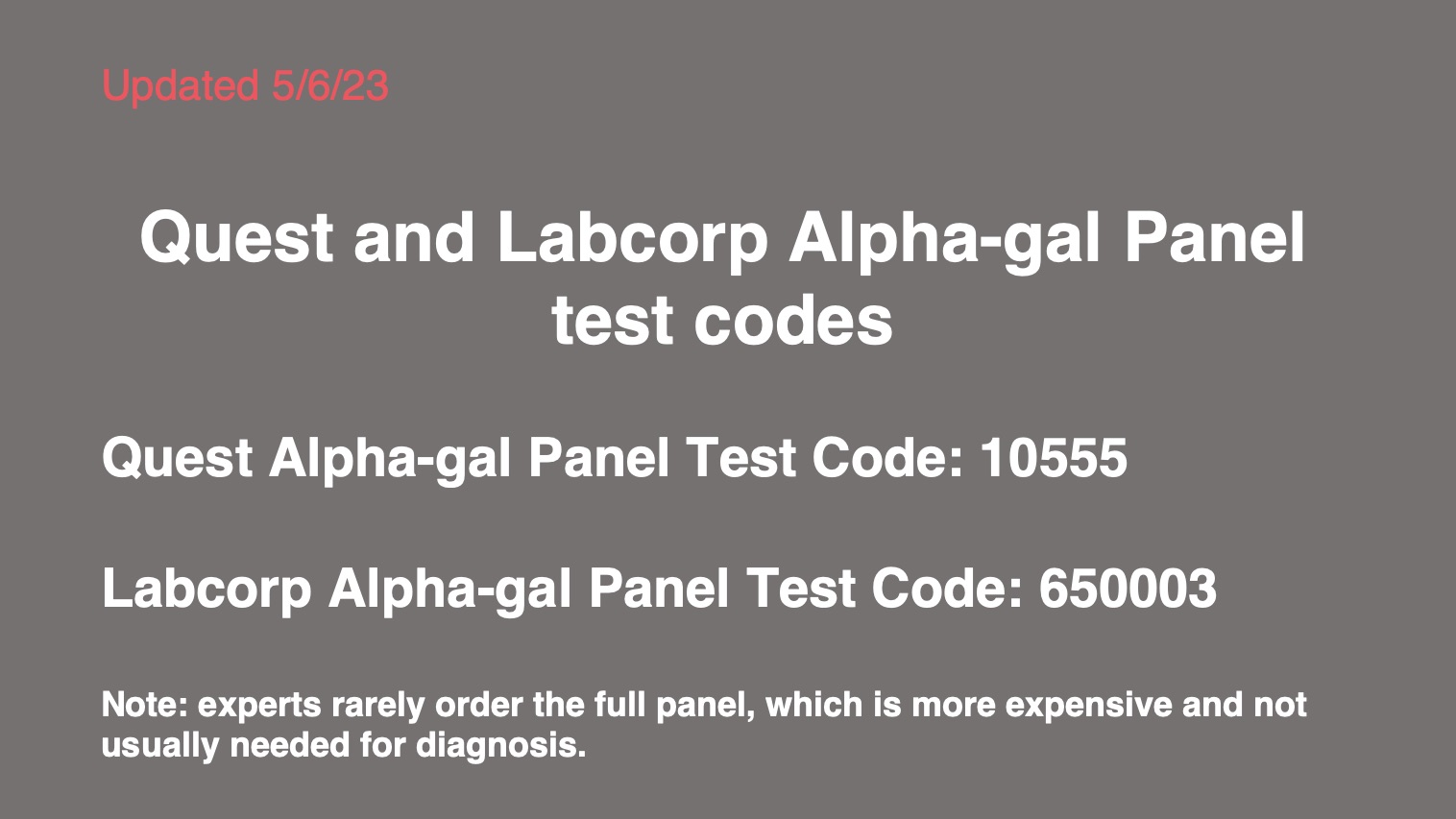
The Alpha-gal Panel
Sometimes healthcare providers order the alpha-gal IgE test as part of an Alpha-gal Panel that includes tests for beef, pork, and lamb as well. Sometimes milk is also included.
- The advantage of ordering these additional tests is that they can be helpful for figuring out whether a patient has a mammalian meat allergy other than AGS when the test for alpha-gal IgE is negative.
- The disadvantages of the panel are:
- The panel is considerably more expensive than the test for alpha-gal IgE alone.
- The results can lead to confusion. See What Do My Test Results Mean?
- Experts do not recommend the routine use of the full Alpha-gal Panel for diagnosis of alpha-gal syndrome (Scott Commins, personal communication).
Viracor (U.S)
Below is Viracor’s information on the Alpha-gal Panel.
- Alpha-Gal Panel
Test Code: 403196P
Tests in this Panel:
*Galactose-alpha-1,3 galactose (Alpha-Gal) IgE
*Beef (Bos spp) IgE
*Pork (Sus spp) IgE
*Lamb / Mutton (Ovis spp) IgE
Quest and Labcorp (U.S.)
When Your Doctor Won’t Order the Test
Sometimes healthcare providers refuse to order the test for alpha-gal IgE, even when a patient has a compelling clinical history.
- Often this is because they are either unfamiliar with AGS or the full spectrum of symptoms with which it manifests.
- Sometimes it may be that they can’t find the codes.
It’s always best to work with a healthcare provider, and patients should not self-diagnose, but in some cases, frustrated patients resort to getting tested without the support of a healthcare provider.
The following lab will test you for alpha-gal IgE without a doctor’s orders. Note that they charge more than you would pay with an order from a doctor.
If you order your own test and test positive, be sure to schedule a follow up appointment with an allergist, so they can help you figure out what the test results mean and how you should proceed.
Patel and Iweala write:
Some test sites include alpha-gal-specific IgE testing within an ‘alpha-gal panel’, which also includes beef, mutton/lamb, pork, and cow’s milk specific IgE testing as patients allergic to alpha-gal frequently have specific IgE that binds to multiple mammal-derived allergens, presumably binding to alpha-gal glycans rather than peptide epitopes. This testing, in conjunction with testing for IgE to cat and dog aeroallergens, serves as a crude surrogate to confirm alpha-gal syndrome if alpha-gal-specific IgE testing is not readily available. However, the alpha-gal-specific IgE and total IgE levels are the most useful serologic tests for confirming the diagnosis of alpha-gal syndrome (5).
Total IgE
Some physicians also order a test for total IgE , as in some cases the ratio of alpha-gal IgE to total IgE is clinically significant (1), especially in nonatopic patients with low total IgE.
Expert Thomas Platts-Mills, et al write:
If the antibodies are greater than or equal to 2 IU/mL or more than 2% of the total IgE, this makes the diagnosis very likely. We often measure total IgE because some cases are nonatopic and have low total IgE. Recently, we saw a case with a convincing history whose total serum IgE was 6.0 IU/mL and sIgE to α-Gal was 0.8 IU/mL. Thus, although the sIgE was less than 1.0 IU/mL, it was nonetheless more than 10% of the total IgE (1).
Other Tests
- Sometimes tests for milk and gelatin allergy are also ordered.
- The results of milk and gelatin tests can lead to confusion and are not routinely recommended (Scott Commins, personal communication).
- See What Do My Test Results Mean?
- Basal serum tryptase levels may be measured as a surrogate for mast cell burden (5).
Commins writes:
The carbohydrate moiety alpha-gal is found in mammalian milk, as evidenced by the positive immunoassay results to cow’s milk. Consistent with prior studies, 11 of 12 subjects had negative immunoassay results to the casein component of cow’s milk, suggesting that this milk protein antigen is not a significant site of alpha-gal–based glycosylation (3).
Patel and Iweala write:
We also check basal serum tryptase levels, as a surrogate for mast cell burden, particularly in those who present with anaphylaxis. Just as anaphylaxis to stinging insect venom can unmask an underlying systemic mastocytosis, individuals with alphagal syndrome have also been subsequently diagnosed with indolent systemic mastocytosis (ISM) (5).
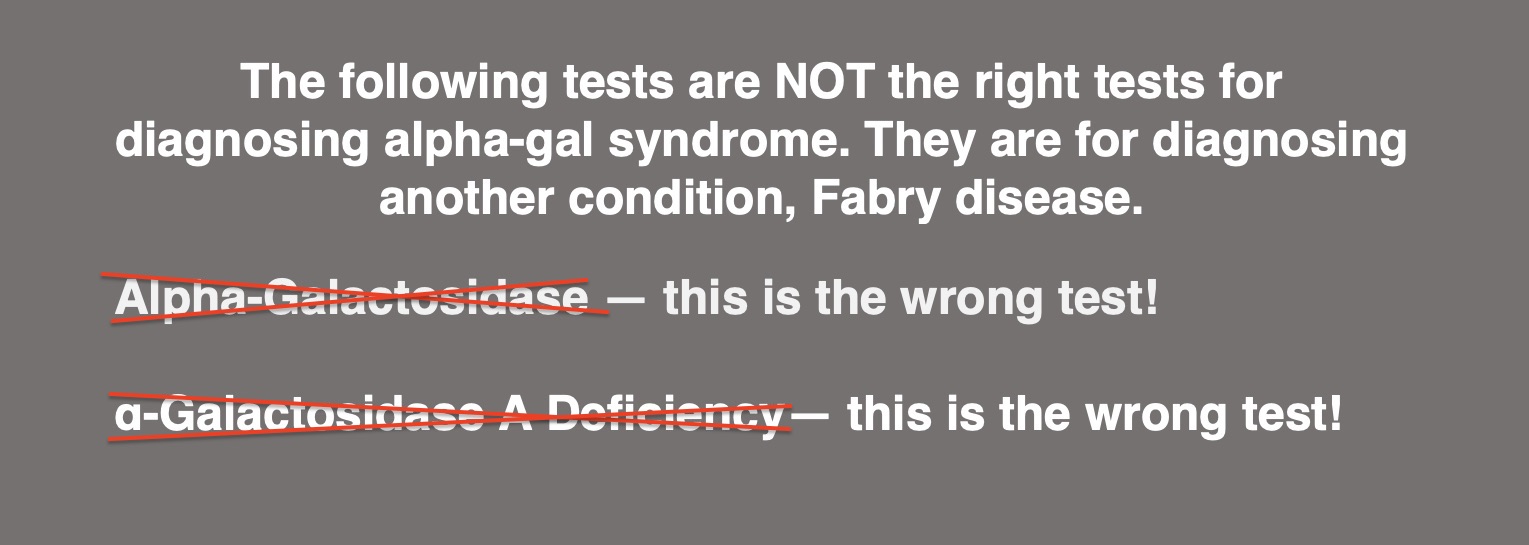
The WRONG Test
Unfortunately, very often the wrong blood test is performed. The test below is NOT the right test for diagnosing alpha-gal syndrome. It’s for diagnosing another condition, Fabry disease.
- Alpha-Galactosidase — this is the wrong test!
- α-Galactosidase A Deficiency— this is the wrong test!
- The main reasons why this test is sometimes mistakenly ordered are:
- Even though a-galactosidase has nothing to do with alpha-gal syndrome, the names sound similar
- Doctors and laboratory staff have trouble finding the correct test codes
- You can help prevent this problem by bringing a copy of the correct test codes to both your doctor’s appointment and to the lab where you have your blood drawn. These are provided in the PDF below, which you can download and print.
- Ask your doctor for a copy of your lab report, both for your records and so you can make sure the right test was ordered.
Here are the correct codes, as of May 6, 2023. You can print this PDF and take it to your doctor’s appointment.
CLICK HERE TO DOWNLOAD A PDF WITH TEST CODES FOR BOTH ALPHA-GAL IGE AND THE ALPHA-GAL PANEL
My allergist ordered the right test for the allergy to Alpha-gal, but the lab tech in the hospital couldn’t find a code for it, so when the test came back positive, the lab tech coded me positive for Fabry disease.
I was given the wrong test. It took 3 different labs to finally get it right. When my dr got the results of the wrong test (for fabry) he read it and said nope you don’t have ag. I had to correct him.
My husband’s allergist ran the wrong test.
I was given the wrong test (alpha-galactosidase)
No! Wrong test!
A Warning about Gelatin
Parenteral administration of medical products that contain bovine or porcine gelatin is considered even more risky for patients with AGS than consumption of red meat (15). This risk is not ruled out by negative results for sIgE to gelatin. Individuals who are sensitized to alpha-gal may experience anaphylactic reactions to parenterally administered gelatin despite testing negative for sIgE to gelatin (16).
Bakhtiar, et al write:
It appears that the diagnosis of alpha‐gal‐related gelatin sensitisation and allergy may readily be missed by a conventional gelatin sIgE assay. Possibly, the allergenic target for the gelatin immunoassay does not include the alpha‐gal moiety (16).
Prepare for Your Appointment
You may want to bring the following information to your first appointment with an allergist:
Test results
Relevant test results, including the results of any:
- Allergy testing
- Tick-borne disease testing
- Labwork from your most recent annual check-up
Notes about tick exposure
- Do you hike, hunt, bird, garden, or have other hobbies that involve lots of time outdoors?
- Are you a field biologist, farmer, forester, park ranger, or have another job that involves working outdoors?
- Have you ever had a tick bite? If so:
- How many tick bites?
- When were you bitten? If you don’t remember a date, what time of year was it?
- Do you know ID what species the tick was? Bring photos if you them!
- Were you diagnosed with any tick-borne diseases?
- Did you have any irritation at the site of the tick bite, like itching or redness? If so, how long did it last?
- Have you ever had any chigger bites?
Notes about your symptoms
Symptoms
Include information about the following symptoms and any other symptoms you have experienced
- Classic allergic symptoms, including any rashes, swelling, dizziness, low blood pressure, difficulty breathing, loss of consciousness etc.
- Gastrointestinal symptoms, like pain, cramping, diarrhea, vomiting, or heartburn
- Joint pain/arthritis
- If you have photos of your reactions, bring them.
- Include information about the date and time of the symptoms, if you remember
Foods
- Include information about any foods you ate within ten hours prior to developing symptoms.
- Note how soon after eating these foods your symptoms developed.
Medications/medical products
- Bring a written list of any medications and/or supplements that you take.
- Note any adverse reactions you have had to medications, vaccines, or other medical products.
Information about alpha-gal syndrome
Unless you are seeing an expert, consider bringing these papers. They were written by experts on alpha-gal syndrome and include information that your healthcare provider may find useful:
- Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients
- Diagnosis and management of patients with the α-Gal syndrome
- Ask your doctor if they have access to Up-to-Date. If they do, recommend that they read the article on meat allergies, which is written by Scott P. Commins, MD, PhD, a leading expert on AGS.
Other helpful information
The summary in the below PDF includes basic information about testing, test codes, and the ICD code (helpful for insurance).
It took 2 weeks to get diagnosed. My doctor told me there was no way I had alpha-gal syndrome, and said he was only running the test to prove me wrong.
What Do My Test Results Mean?
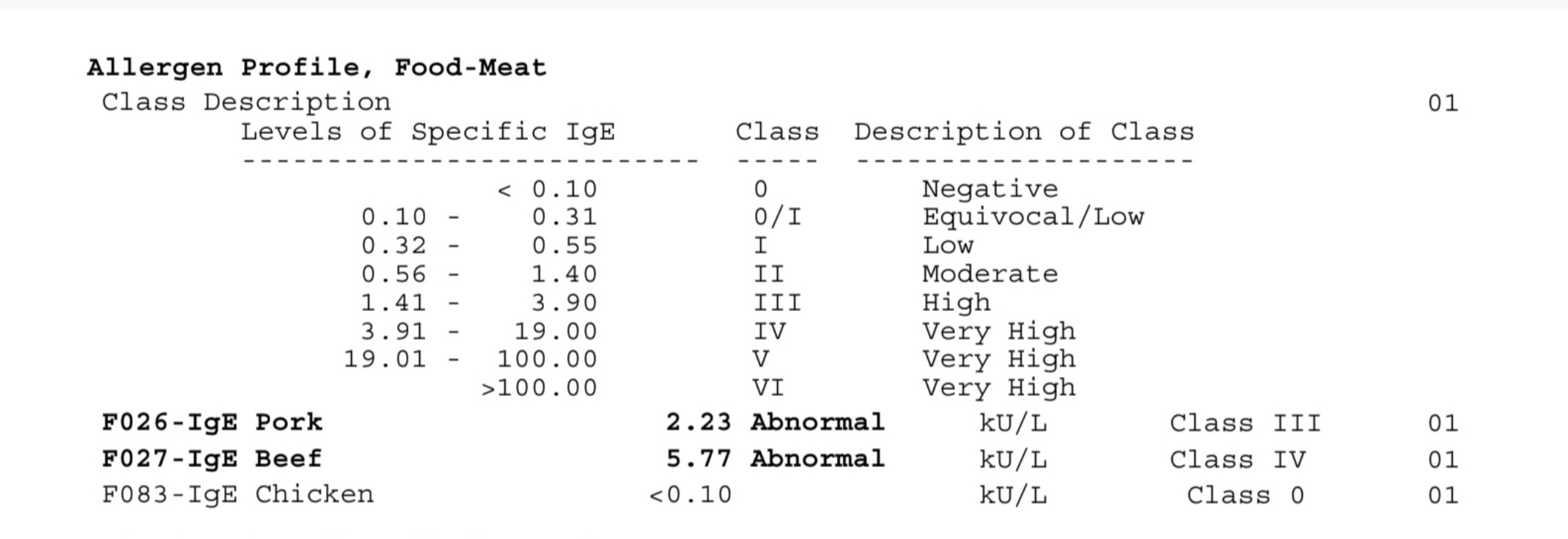
Your lab report may include some or all of the following test results
Galactose-alpha-1,3-galactose IgE
- This is a measure of your galactose-alpha-1,3-galactose (or alpha-gal for short) specific IgE antibodies.
Pork IgE and Beef IgE
- These are measures of your IgE antibodies to the proteins in beef and pork.
- The samples used to perform these tests may contain both proteins and alpha-gal.
Total IgE
- This is a measure of all your IgE antibodies to all allergens, not just to one specific allergen.
What the test results mean
You need to ask your doctor what the numbers in your lab report mean. We are not qualified to interpret them for you. However, the following guide may help you talk to your doctor about your results.
Galactose-alpha-1,3-galactose IgE and Total IgE
- At the time this is being written, antibody levels > 0.10 kU/L are typically considered a positive test result (10).
- Antibody levels >2 IU/ml or >2% of total IgE make the diagnosis of alpha-gal syndrome very likely (1).
- Physicians at UVA recently saw a case with a convincing history whose total serum IgE was 6.0 IU/ml and alpha-gal IgE was 0.8 IU/ml. Thus, although the sIgE was < 1.0 IU/mL it was nonetheless > 10% of the total IgE. (1)
- Only 1-8% of individuals who are sensitized to alpha-gal have clinical alpha-gal syndrome (2). This means that many people who test positive for alpha-gal IgE do not seem to exhibit symptoms after eating red meat. As reactivity to alpha-gal appears to occur on a spectrum, a portion of these people may react to some medications or medical products containing alpha-gal (11) and/or experience symptoms after eating mammalian organs, which contain more alpha-gal than mammalian muscle. (12)
- As with any allergy, false negatives also occur, although they are less common.
- Anecdotal reports from people with AGS seem to suggest that a not insignificant number of people who are initially seropositive for alpha-gal IgE eventually revert to seronegative but continue to experience reactions.
Pork IgE and Beef IgE
If you test positive for pork and/or beef IgE it may mean:
- You are allergic to proteins in pork and/or beef. For example if you test positive for beef IgE you may have what is called “primary beef allergy.” It’s a different allergy than alpha-gal syndrome, but both make you allergic to beef.
OR
- You are not allergic to proteins in pork or beef. You have alpha-gal syndrome. You tested positive because the test samples contain alpha-gal in addition to proteins. This is very common, especially with the beef test.
OR
- Some people who test negative for alpha-gal and beef IgE, but positive for pork IgE, may have pork-cat syndrome, which is an allergy to a protein found in both cats and pork. (13).
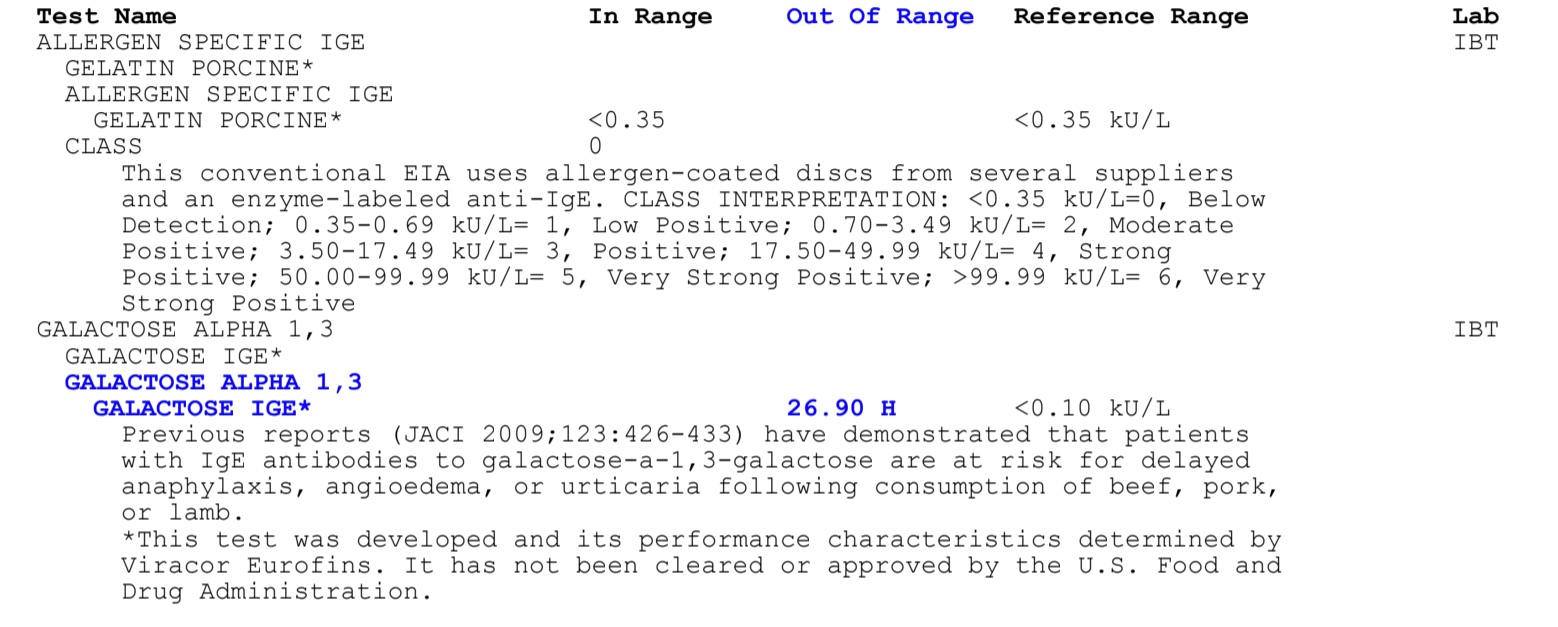
Example:
See below two sets of test results. These are from a real patient.
Clinical History
The patient has a clinical history of:
- Multiple tick bites
- Delayed allergic reactions to beef, pork, dairy, gelatin, dairy, mammalian byproducts in both food and medications, and carrageenan.
- These reactions began a few weeks after the tick bites
- Symptoms include hives, angioedema, anaphylaxis, and abdominal pain occurring 1-10 hours after ingestion of meat and other foods with ingredients derived from mammals
How these results were interpreted:
- The elevated galactose-α-1,3-galactose (alpha-gal) IgE levels and the ratio of galactose-α-1,3-galactose (alpha-gal) IgE to total IgE in conjunction with the patient’s clinical history suggest that the patient has alpha-gal syndrome.
- The elevated pork and beef IgE do not mean that the patient is allergic to beef and pork proteins. Most likely, alpha-gal in the beef and pork samples used for the test produced the positive results. This is common. Since the patient tests positive for alpha-gal IgE and has delayed reactions after ingesting mammalian meat, these test results don’t have much meaning. Regardless of whether they tested positive or negative for beef and pork protein IgE, they are allergic to alpha-gal in beef and pork.
- The negative result for porcine gelatin means that the patient is not allergic to the protein in porcine gelatin. However, since the patient tests positive for alpha-gal, which is also in gelatin, they may also react to gelatin. Studies show that patients who are allergic to alpha-gal may have anaphylactic reactions to both ingested and parenterally administered gelatin.
What is this patient allergic to?
- This patient is not allergic to proteins in porcine gelatin and likely is also not allergic to any proteins in meat.
- This patient is allergic to galactose-α-1,3-galactose (alpha-gal) which is found in all mammalian cells, tissues, and fluids including all mammalian meats, dairy, and gelatin.
- Despite testing negative for IgE to gelatin, this patient reacts to even small amounts of gelatin in foods and medications.
Does my galactose-alpha-1,3-galactose (alpha-gal) IgE level tell me how reactive I will be to alpha-gal?
No. This number does not tell you how reactive you will be to foods, drugs, or other products with alpha-gal in them. It is only useful for predicting whether you will react to them at all.
- Some people with high levels of alpha-gal IgE are not very reactive to it.
- Some people with low levels of alpha-gal IgE are very reactive to it.
- Researchers are studying whether the ratio of alpha-gal IgE/total IgE is correlated with how reactive to alpha-gal people are, but the results of this research have not yet been published.
I don’t know if I would call it a true false positive or a subclinical positive (14).
References–in development
1. Platts-Mills TA, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the α-Gal syndrome. The Journal of Allergy and Clinical Immunology: In Practice. 2020 Jan 1;8(1):15-23.
2. Commins SP. Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients. Expert Review of Clinical Immunology. 2020 Jul 9:1-1.
3. Commins SP, James HR, Stevens W, Pochan SL, Land MH, King C, Mozzicato S, Platts-Mills TA. Delayed clinical and ex vivo response to mammalian meat in patients with IgE to galactose-alpha-1, 3-galactose. Journal of allergy and clinical immunology. 2014 Jul 1;134(1):108-15.
4. Mehlich J, Fischer J, Hilger C, Swiontek K, Morisset M, Codreanu-Morel F, Schiener M, Blank S, Ollert M, Darsow U, Biedermann T. The basophil activation test differentiates between patients with alpha-gal syndrome and asymptomatic alpha-gal sensitization. Journal of Allergy and Clinical Immunology. 2019 Jan 1;143(1):182-9.
5. Patel C, Iweala OI. ‘Doc, will I ever eat steak again?’: diagnosis and management of alpha-gal syndrome. Current Opinion in Pediatrics. 2020 Sep 29.
6. Fischer J, Hebsaker J, Caponetto P, Platts-Mills TA, Biedermann T. Galactose-alpha-1, 3-galactose sensitization is a prerequisite for pork-kidney allergy and cofactor-related mammalian meat anaphylaxis. Journal of allergy and clinical immunology. 2014 Sep 1;134(3):755-9.
7. Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, Kocan KM, Fahy JV, Nganga LW, Ronmark E, Cooper PJ. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1, 3-galactose. Journal of Allergy and Clinical Immunology. 2011 May 1;127(5):1286-93.
8. Caponetto P, Fischer J, Biedermann T. Gelatin-containing sweets can elicit anaphylaxis in a patient with sensitization to galactose-α-1, 3-galactose. The Journal of Allergy and Clinical Immunology: In Practice. 2013 May 1;1(3):302-3.
9. Van Nunen SA, O’Connor KS, Clarke LR, Boyle RX, Fernando SL. An association between tick bite reactions and red meat allergy in humans. The Medical journal of Australia. 2009 May 4;190(9):510-1.
10. Viracor
11. Chung, C. H., et al. (2008). Cetuximab-Induced Anaphylaxis and IgE Specific for Galactose-α-1,3-Galactose. N Engl J Med 2008; 358:1109-1117
12. Fischer, J. and T. Biedermann (2016). “Delayed immediate-type hypersensitivity to red meat and innards: current insights into a novel disease entity.” Journal Der Deutschen Dermatologischen Gesellschaft 14(1): 38-43.
13. Posthumus, J. et al. (2013). “Initial Description of Pork-Cat Syndrome in the United States ” The Journal of allergy and clinical immunology vol. 131,3 : 923-5.
14. McGintee, E. (2015). “Meat Allergy Triggered by a Tick Bite with Erin McGintee, MD.” Video-taped lecture. Retrieved from https://youtu.be/hj96Vvr1WhQ.
15. Fischer J, Huynh HN, Hebsaker J, Forchhammer S, Yazdi AS. Prevalence and Impact of Type I Sensitization to Alpha-Gal in Patients Consulting an Allergy Unit. International Archives of Allergy and Immunology. 2020;181(2):119-27.
16. Bakhtiar MF, Leong KW, Kwok FY, Hui MT, Tang MM, Joseph CT, Bathumana‐Appan PP, Nagum AR, ZHM Y, Murad S. P66: ALLERGIC REACTION TO BOVINE GELATIN COLLOID: THE ROLE OF IMMUNOGLOBULIN E TOWARDS GALACTOSE‐ALPHA‐1, 3‐GALACTOSE: IMPLICATIONS BEYOND RED MEAT ALLERGIES. Internal Medicine Journal. 2017 Sep;47:24-.
17. Wilson JM, Platts-Mills TA. Red meat allergy in children and adults. Current opinion in allergy and clinical immunology. 2019 Jun 1;19(3):229-35.
18. Wilson JM, Schuyler AJ, Workman L, Gupta M, James HR, Posthumus J, McGowan EC, Commins SP, Platts-Mills TA. Investigation into the α-gal syndrome: characteristics of 261 children and adults reporting red meat allergy. The Journal of Allergy and Clinical Immunology: In Practice. 2019 Sep 1;7(7):2348-58.
19. Werfel SJ, Cooke SK, Sampson HA. Clinical reactivity to beef in children allergic to cow’s milk. Journal of Allergy and Clinical Immunology. 1997 Mar 1;99(3):293-300.
20. Fiocchi A, Restani P, Riva E. Beef allergy in children. Nutrition. 2000 Jun 1;16(6):454-7.
21. Martelli A, De Chiara A, Corvo M, Restani P, Fiocchi A. Beef allergy in children with cow’s milk allergy; cow’s milk allergy in children with beef allergy. Annals of Allergy, Asthma & Immunology. 2002 Dec 1;89(6):38-43.
22. Drouet M, Boutet S, Lauret MG, Chène J, Bonneau JC, Le Sellin J, Hassoun S, Gay G, Sabbah A. The pork-cat syndrome or crossed allergy between pork meat and cat epithelia (1). Allergie et immunologie. 1994 May;26(5):166.
23. Posthumus J, James HR, Lane CJ, Matos LA, Platts-Mills TA, Commins SP. Initial description of pork-cat syndrome in the United States. Journal of Allergy and Clinical Immunology. 2013 Mar 1;131(3):923-5.
All the information on alphagalinformation.org is provided in good faith, but we, the creators and authors of the Alpha-gal Information website offer no representation or warranty, explicit or implied, of the accuracy, adequacy, validity, reliability, availability, or completeness of any information on this site. Under no circumstances should we have any liability for any loss or damage incurred by you as a result of relying on information provided here. We are not physicians or medical professionals, researchers, or experts of any kind. Information provided in this website may contain errors and should be confirmed by a physician. Information provided here is not medical advice. It should not be relied upon for decisions about diagnosis, treatment, diet, food choice, nutrition, or any other health or medical decisions. For advice about health or medical decisions including, but not limited to, diagnosis, treatment, diet, and health care consult a physician.
READ FULL DISCLAIMER>